Brain-Machine Tech Helps Relieve Mysterious 'Phantom Limb Pain'

A new treatment appears to help relieve the "phantom limb pain" that people who have undergone amputations or have paralysis in a limb sometimes experience, a new study from Japan finds.
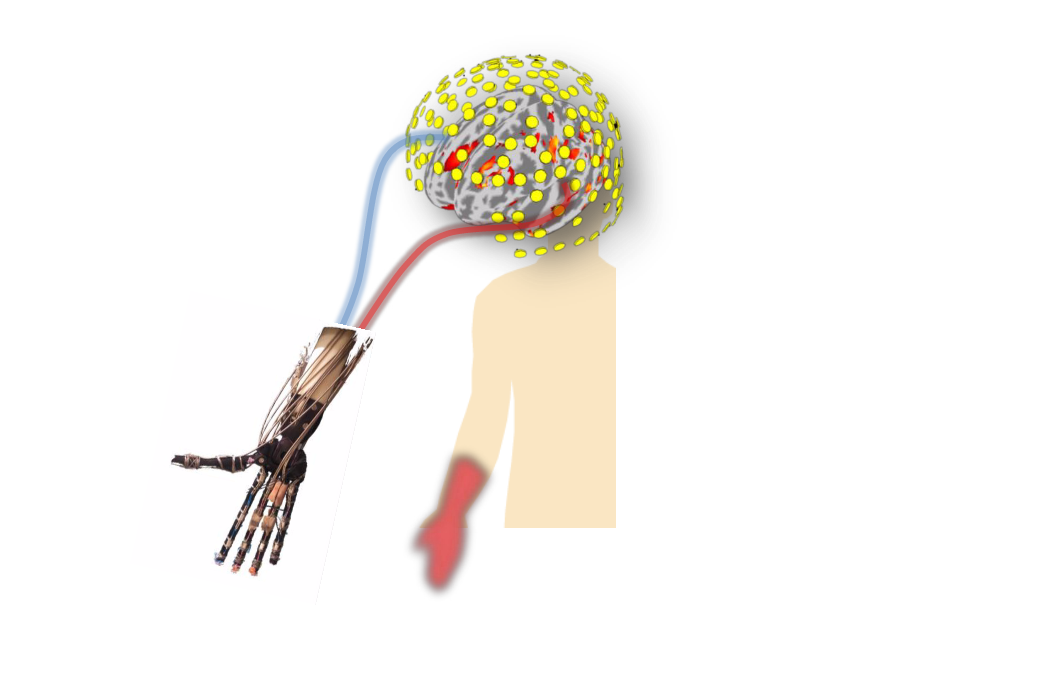
In the study, the researchers used brain-machine-interface technology to treat patients who had phantom limb pain, which means they experience pain in a missing or paralyzed limb.
The technology records a person's brain activity, and then translates that activity into the movement of a robotic prosthesis, according to the study, published today (Oct. 27) in the journal Nature Communications.
If someone had phantom limb pain in a hand, "even though the hand is gone, people with phantom limb pain still feel like there's a hand there — it basically feels painful, like a burning or hypersensitive type of pain, and conventional painkillers are ineffective in treating it," Dr. Ben Seymour, a neuroscientist at the University of Cambridge in England and a co-author of the study, said in a statement.
Normally, a person's brain generates activity to move a body part, said Dr. Takufumi Yanagisawa, an assistant professor of neurosurgery at Osaka University in Japan and the lead author of the study. [10 Things You Didn't Know About the Brain]
Then, as the person moves that body part, the brain takes in sensory information to check that the movement is occurring as the person intends it to, Yanagisawa told Live Science. This includes not only visual information from the eyes (as they watch the body part move) but also information from the limb itself about any touch sensations it experiences as it moves and information about where the body part is in space that comes to the brain from the muscles, he said.
When a person with phantom limb pain tries to move a body part, the brain generates the same activity to move that body part, but it never receives the sensory information confirming that the movement was successful, Yanagisawa said. This discrepancy — between the intention to move and the actual results — are thought to be the source of phantom limb pain, he said.
Get the world’s most fascinating discoveries delivered straight to your inbox.
Fixing phantom limb pain
Previously, scientists thought that simulating the movement of the "phantom" body part, by using a robotic prosthesis, for example, would relieve the pain, Yanagisawa said.
But in the new study, when the researchers tried this, using the brain-machine-interface technology with 10 patients, they found that it had the opposite effect: It made the patients' pain worse, Yanagisawa said.
It's possible that the movement of the robotic prosthesis didn't get rid of the discrepancy between the intent to move and the sensory feedback the brain received, the researchers wrote in the study. Although the patients saw the prosthesis move, they still could not feel it or get the sensory information from the muscles about where the limb was in space, the researchers said. [10 Technologies That Will Transform Your Life]
The researchers tried a different approach with these same patients. They asked the patients to try moving a phantom hand on the other side of the body from where they were experiencing the pain. In other words, if a patient's left hand was paralyzed or amputated, the researchers told the patient to imagine he or she had a phantom hand on the right, and to try moving the right phantom hand instead.
Using the brain-machine-interface technology, the researchers recorded the brain activity generated when the patients tried to move a phantom limb on the "wrong" side of the body, and translated this activity into the movement of the robotic prosthesis.
This time, the patients' phantom pain decreased.
Why it works
It's possible that by training the "wrong" side of the body, the patients avoided the discrepancy in their brain between the movement and the sensory information that came back. In other words, the patients' brains weren't waiting for sensory information from the phantom hand, but rather from the other hand.
The researchers noted, however, that the technology isn't ready for widespread use.
The pain-relieving results were temporary, Seymour said.
In addition, the treatment currently requires a large and expensive piece of medical equipment in order to work, Seymour said.
Originally published on Live Science.

 Live Science Plus
Live Science Plus