Mpox (monkeypox): Symptoms, pictures, treatments & vaccines
Mpox is a viral disease.
Get the world’s most fascinating discoveries delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?
Join the club
Get full access to premium articles, exclusive features and a growing list of member rewards.
Mpox, formerly known as monkeypox, is a disease caused by the mpox virus, a pathogen closely related to variola virus, which causes smallpox. Mpox and smallpox infections trigger similar symptoms, but mpox tends to be far milder by comparison.
Why is there a new name for monkeypox?
On Nov. 28, 2022, the World Health Organization (WHO) announced that the agency would be phasing out use of the term "monkeypox" and instead call the virus and the disease it causes "mpox."
During the 2022 mpox outbreak, various scientists and public officials raised concerns that the previous name erroneously suggested that monkeys serve as the primary mpox reservoir in the wild and the main source of mpox infections in people. In reality, rodents are likely the main reservoir of the virus and the pathogen can jump to and spread between people via various routes.
Experts also argued that the term "monkeypox" unnecessarily linked the virus to Africa, and by extension, fed into the idea that the disease is exclusive to Africa and to African people. "Monkey" has also long been used as a racial slur against Black people, furthering the stigmatizing potential of the term.
In line with the shift to "mpox" over "monkeypox," in August 2022, the WHO also renamed the two major clades, or related groups, of mpox viruses. They were previously known as the "Congo Basin" or "Central African" clade and the "West African" clade, and now, they're called Clade I and Clade II.
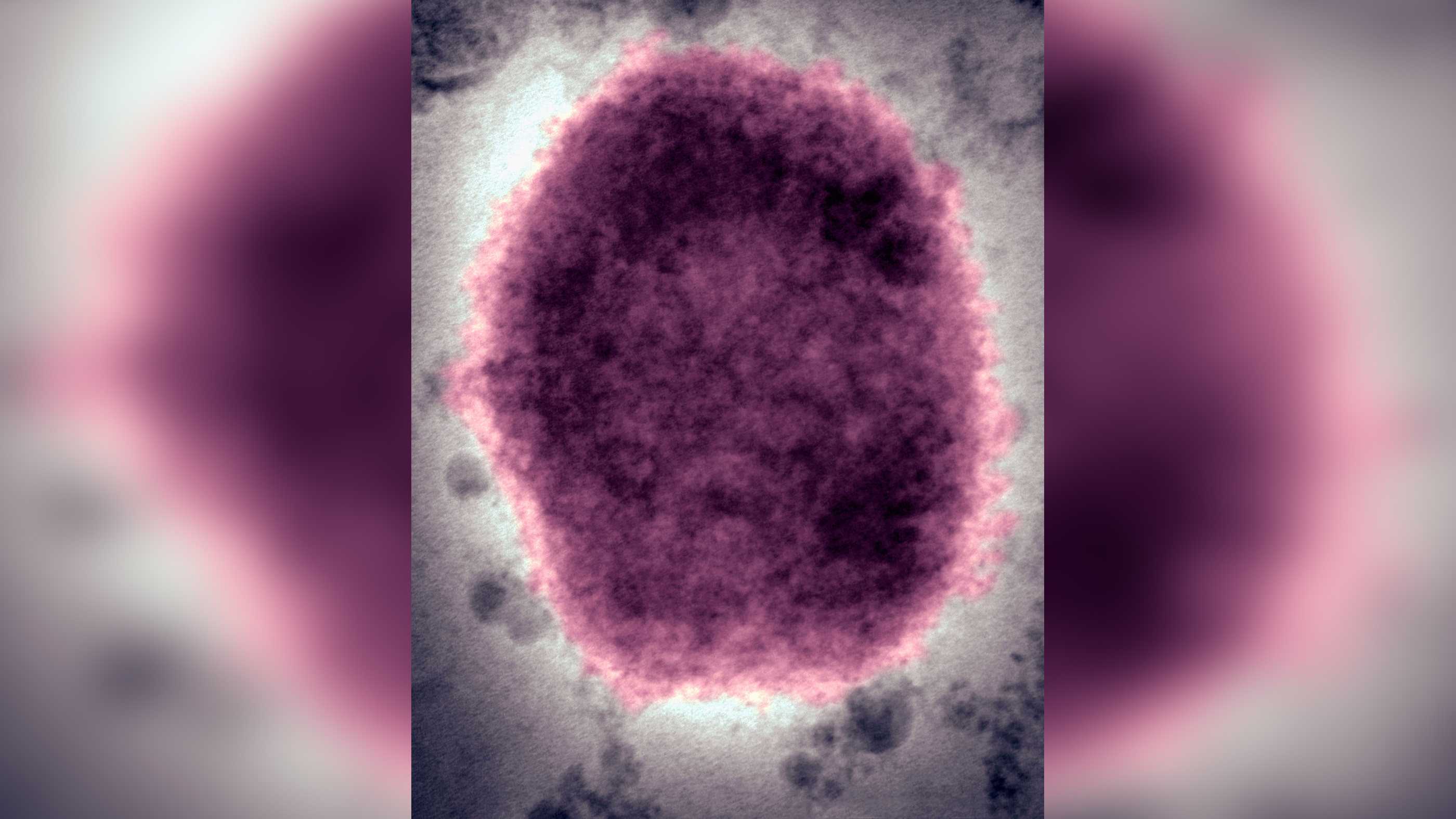
What is the mpox virus?
The mpox virus belongs to the Orthopoxvirus genus within the Poxviridae family of viruses. Other viruses in the Orthopoxvirus genus include the viruses that cause variola (smallpox), cowpox and camelpox, according to the Centers for Disease Control and Prevention (CDC).
According to the World Health Organization (WHO), there are two distinct clades — or genetically related groups — of mpox viruses: Clade I and Clade II. Evidence suggests that Clade I is more likely to cause severe and fatal disease, and also may be more transmissible, than Clade II.
Get the world’s most fascinating discoveries delivered straight to your inbox.
Mpox was first discovered in 1958, when laboratory monkeys at the Statens Serum Institute in Copenhagen, Denmark, came down with a pox-like illness, according to the WHO. The first known human case was identified in 1970 in a 9-month-old boy living in the Democratic Republic of the Congo.
Despite the virus's name, monkeys and other nonhuman primates are likely not the pathogen's main hosts, although this still needs to be confirmed, according to the WHO. Rather, rodents are thought to be the natural reservoir for the mpox virus in the wild. Although primates, including humans, are susceptible to the virus, they are incidental hosts, meaning they can become infected but don't serve as a constant "reservoir" for the virus.
Among African rodents, mpox infection has been documented in rope squirrels, tree squirrels, Gambian pouched rats and dormice. And in 2003, scientists learned that prairie dogs are also susceptible to mpox infection, after prairie dogs in the U.S. caught the virus, according to the CDC. The prairie dogs had been housed near imported small mammals from Ghana, including several rodent species that were later found to be infected with mpox. The prairie dogs were sold as pets and ended up spreading the mpox virus to dozens of people in six states.
Where does mpox spread?
Mpox regularly circulates in several Central and West African countries, meaning the disease is "endemic" in those areas. Those countries include the Democratic Republic of the Congo, the Republic of the Congo, Nigeria, the Central African Republic, Cameroon, Côte d'Ivoire, Gabon, Liberia, Sierra Leone and Sudan, according to the CDC.
The 2003 mpox outbreak in the U.S. marked the first time that human cases of mpox had been reported outside of Africa, the CDC states. Between 2003 and 2022, cases of mpox had been reported sporadically in non-endemic countries — including the United Kingdom, Israel and Singapore — but the majority of these cases were linked to travel to an endemic country or exposure to imported animals from an endemic country.
Then, in 2022, mpox began spreading in non-endemic countries at unprecedented levels. The first cases were detected in London in May, and by mid-July, more than 16,000 cases had been reported in 75 countries and territories; the scale of the spread prompted the WHO to declare the outbreak a public health emergency of international concern.
What are the symptoms of mpox?
The incubation period for mpox — or the time it takes to develop symptoms following an exposure — is roughly one to two weeks. Typically, mpox infections start with flu-like symptoms, including the following:
- Fever
- Headache
- Muscle aches
- Fatigue
- Swollen lymph nodes; this swelling may appear in multiple locations, such as the neck and armpit.
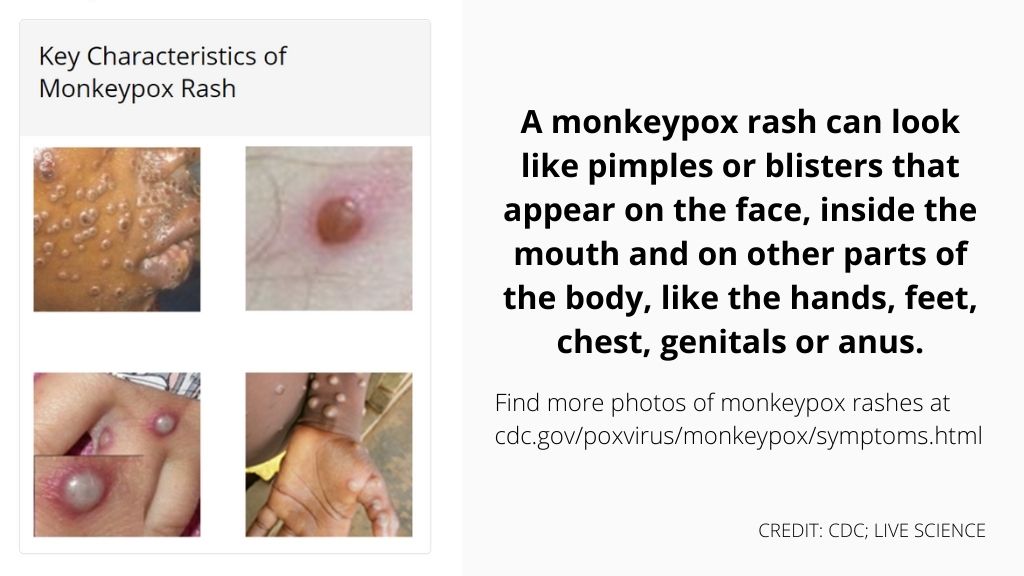
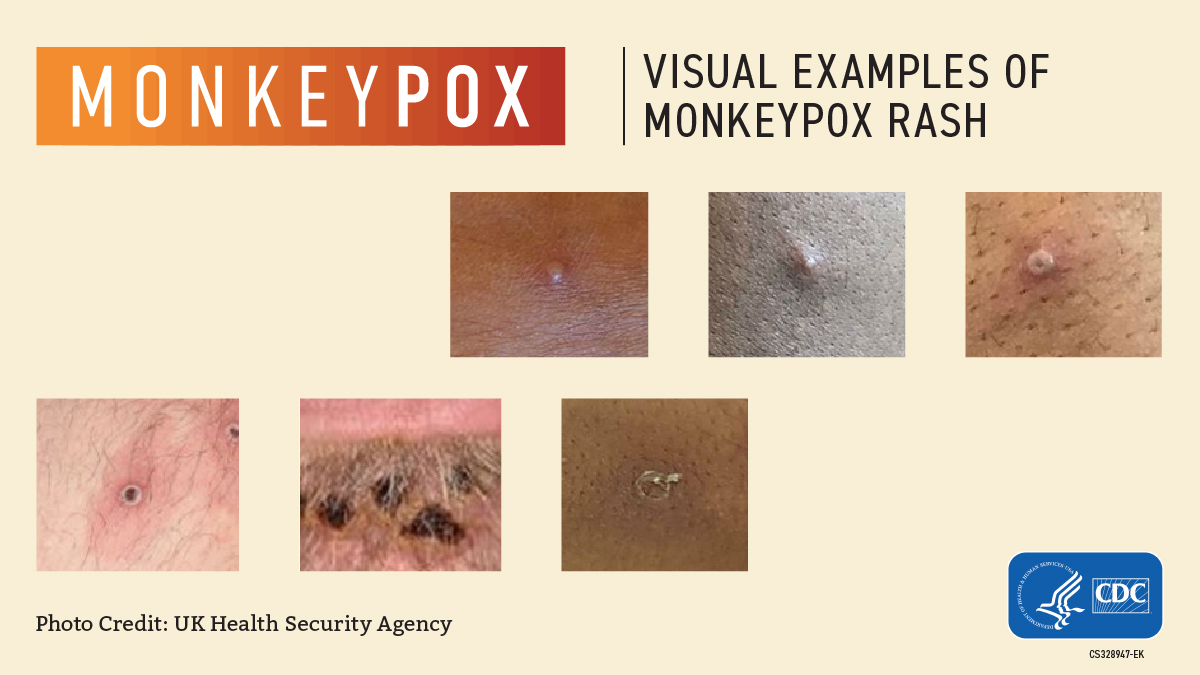
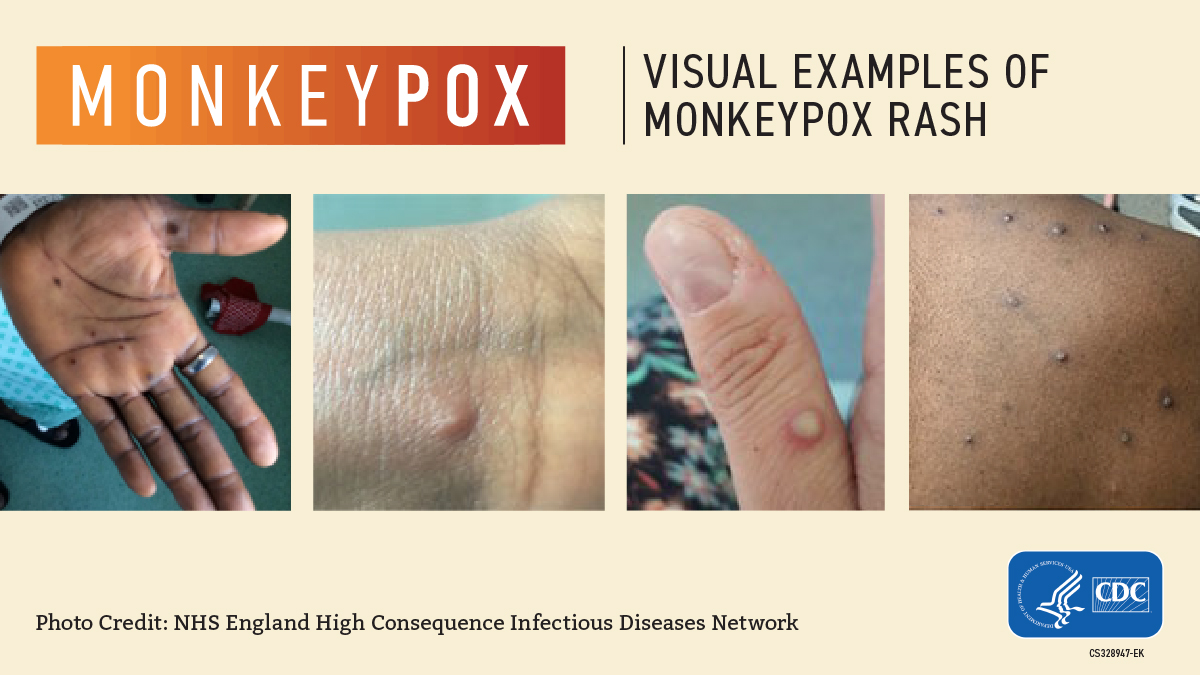
Then, the characteristic "pox" rashes begin to appear, usually around the face and in the oral cavity, and later, on the extremities, including the palms of the hands and soles of the feet. These rashes can resemble those caused by the Varicella zoster virus, which causes chickenpox, and they can also look like those caused by certain sexually transmitted infections, such as syphilis and herpes.
Mpox rashes progress through several stages, starting out as discolored patches of skin and then forming into raised bumps, blisters, and large, pus-filled pimples that eventually scab over and fall off. In severe cases, separate skin rashes can coalesce to form one huge lesion that causes large amounts of skin to slough off at once, according to the WHO.
In the 2022 outbreak, however, some patients' symptoms have diverged from the normal pattern. For example, some patients developed flu-like symptoms after their skin rashes or didn't experience flu-like symptoms at all, the CDC reported in June. Some patients initially developed rashes around the genitals and anus, and these skin lesions caused symptoms of painful inflammation and rectal bleeding. Sometimes, patients have had rashes in different stages of progression at the same body site, which is unusual.
In most cases, the symptoms of mpox remain fairly mild and resolve in two to four weeks. However, some groups — including children younger than 8, people with weakened immune systems or a history of eczema, and people who are pregnant or breastfeeding — face a greater risk of developing severe mpox infections than the general public, according to the CDC.
Mpox infections can sometimes result in severe complications, including secondary infections; inflammation of the air sacs in the lungs (bronchopneumonia); an extreme, full-body immune response (sepsis); inflammation of the brain (encephalitis); and infection of the cornea with ensuing loss of vision, according to the WHO.
Photos of mpox rashes

Is mpox deadly?
Clade I mpox viruses are linked to a higher risk of severe disease and death than those in Clade II. Estimates of the case fatality rate for Clade I range between 6% and 10%, while estimates for Clade II range between 1% and 3.5%, according to the UCLA Fielding School of Public Health.
The 2022 outbreak has been driven by Clade II viruses. As of July 23, when the WHO declared the 2022 outbreak a public health emergency, there were five reported deaths out of more than 16,000 cases, worldwide.
How does mpox spread?
Mpox can spread from animals to humans when people come into contact with the blood, bodily fluids, rashes or sores of infected animals, according to the WHO. People can also catch the virus if they are scratched or bitten by an infected animal, or if they consume undercooked meat or use products made from infected animals, according to the CDC.
Person-to-person mpox transmission can occur when people come into direct contact with an infected person's rashes, scabs or bodily fluids, including pus, mucus and saliva, or with materials contaminated with their bodily fluids, such as clothing or linens, the CDC states. "Direct contact" may include face-to-face, skin-to-skin, mouth-to-mouth or mouth-to-skin contact. It's not yet known whether the virus can spread through semen, vaginal fluids, amniotic fluids, breastmilk or blood, according to the WHO.
In general, the virus typically enters the body through broken skin, the respiratory tract or mucous membranes, which include tissues of the eyes, nose and mouth, according to the UCLA Fielding School of Public Health. In pregnant people, the virus can pass through the placenta to the fetus and also can be transmitted via close contact with newborns during and after birth.
The virus can also spread through respiratory droplets — meaning small drops of saliva and mucus — that are expelled from the mouth and come into contact with the mucus membranes of another person, but this route of transmission typically requires "prolonged" face-to-face contact.
The 2022 mpox outbreak has heavily impacted men who have sex with men, which raised questions (and disinformation) about whether the disease specifically spreads through sexual intercourse.
"While close physical contact is a well-known risk factor for transmission, it is unclear at this time if mpox can be transmitted specifically through sexual transmission routes," according to the WHO. "Studies are needed to better understand this risk." Again, more research is needed to know if the virus spreads through semen or vaginal fluid.
Mpox is much less infectious than its cousin smallpox. The reproduction number, or R-naught (R0), of smallpox is estimated to be between 5 and 7; that means a single infected person would infect five to seven people, on average, Joseph Eisenberg, professor and chair of epidemiology at the University of Michigan, wrote for The Conversation. By comparison, preliminary research suggests that the mpox viruses driving the 2022 outbreak have an R0 of about 0.8, at least among the general public, the WHO reported in June; however, in social networks where the virus is currently more prevalent, the R0 may be greater than 1.
How to prevent mpox transmission
The CDC offers the following tips to prevent the spread of mpox:
- Avoid close, skin-to-skin contact with people who have a rash that looks like mpox.
- Do not touch the rashes or scabs of a person with mpox.
- Do not kiss, hug, cuddle or have sex with someone who has mpox.
- Do not share eating utensils or cups with a person who has mpox.
- Do not handle or touch the bedding, towels or clothing of a person who has mpox.
- Wash your hands often with soap and water, or use an alcohol-based hand sanitizer.
- Within Central and West Africa, avoid contact with animals that can spread the mpox virus, such as rodents and primates. Also avoid sick or dead animals, as well as bedding or other materials they have touched.
What to do if you've been exposed or have symptoms
People who have been exposed to a known mpox case should monitor their symptoms for 21 days following the exposure, the CDC advises. In particular, they should monitor for fever, chills, swollen lymph nodes and new skin rashes. If any of these symptoms develop, these individuals should self-isolate and contact their heath care provider and the local or state health department for further guidance. At that point, individuals may be directed to seek diagnostic testing, and doctors should evaluate whether they're at risk for severe disease or require treatment in a hospital.
People who have recently been exposed to mpox also may be given one of two vaccines — JYNNEOS or ACAM2000 — to reduce the severity of their symptoms or to prevent the illness altogether, according to the CDC. "CDC recommends that the vaccine be given within 4 days from the date of exposure in order to prevent onset of the disease," the agency's website says. "If given between 4–14 days after the date of exposure, vaccination may reduce the symptoms of disease, but may not prevent the disease."
(Note that known contacts of people who've tested positive for mpox may be eligible for vaccination before they develop symptoms, according to the CDC. This is part of a "ring vaccination" strategy, in which close contacts of an initial case are vaccinated to prevent onward transmission of the disease.)
People who test positive for mpox and don't require hospitalization should isolate at home, and when possible, stay in a separate room or area away from people or pets you live with until your symptoms resolve, as it's possible that humans can spread the virus to certain animals, the CDC says. If around others, infected people should wear a mask to prevent the spread of the virus via respiratory droplets, according to Michigan Health.
The WHO also suggests:
- Using a separate bathroom, or cleaning after each use
- Cleaning frequently touched surfaces with soap and water and a household disinfectant and avoiding sweeping/vacuuming (this might disturb virus particles and cause others to become infected)
- Using separate utensils, towels, bedding and electronics
- Doing your own laundry (lift bedding, clothes and towels carefully without shaking them, put materials in a plastic bag before carrying it to the washing machine and wash them with hot water)
- Opening windows for good ventilation
- Encouraging everyone in the house to clean their hands regularly with soap and water or an alcohol-based hand sanitizer.
Is there an mpox vaccine?
Some individuals may be eligible for vaccination against mpox. A vaccine called ACAM2000, originally designed to prevent smallpox, is at least 85% effective at preventing mpox when administered before exposure, the CDC states. In addition, JYNNEOS, a vaccine approved for both smallpox and mpox, is thought to be equally protective against the virus, based on clinical research and animal studies, according to the Johns Hopkins Bloomberg School of Public Health.
People are considered fully vaccinated about two weeks after their second shot of JYNNEOS and four weeks after receiving ACAM2000. As stated in the previous section, the vaccines may be given prior to exposure, to prevent infection, or after exposure to reduce the severity of people's symptoms or to prevent the infection from taking hold.
JYNNEOS is a newer vaccine and generally preferred over ACAM2000, which carries a risk of severe side effects in pregnant people, people with weakened immune systems, and those with certain skin conditions, including atopic dermatitis and eczema, according to the CDC.
Check the CDC website to see if you're eligible for mpox vaccination in the U.S.
Treatments for mpox
There are no drugs specifically approved to treat mpox, and many people recover without the need for specific treatment. However, in severe cases, patients may receive antiviral medications intended to treat other infections; for example, they may receive tecovirimat (brand name TPOXX), which is designed to treat smallpox and also works against other orthopoxviruses, according to the CDC.
Severe mpox infections also may be treated with Vaccinia Immune Globulin Intravenous (VIGIV), which contains antibodies taken from the blood of people who were immunized with the smallpox vaccine.
And as stated above, people who have recently been exposed to mpox also may be given a JYNNEOS or ACAM2000 vaccine to reduce the severity of their symptoms or to prevent the illness altogether, according to the CDC.
2022 mpox outbreak
In early May 2022, health officials in the U.K. reported several mpox cases in London and nearby areas, only one of which was linked to international travel. The case count in the U.K. then began to swell as officials in other European countries flagged their own cases, and the first cases in Canada and the U.S. were identified in mid-May.
More and more countries reported their own cases, and on July 23, the WHO declared the global outbreak to be a public health emergency of international concern. By that point, more than 16,000 cases had been reported in 75 countries and territories.
According to WHO data, the global rate of new mpox cases reached a peak in July and August and generally declined thereafter. As of Dec. 1, some countries continued to report new cases but were seeing much lower rates of illness than they did in late summer.
Check the CDC website for the current global and U.S. case counts.
At the start of the outbreak, cases predominantly appeared among gay men, bisexual men and other men who have sex with men. This epidemiological trend doesn't mean that men who have sex with men are more prone to mpox infection, however; anyone, regardless of sexual orientiation or behavior, can catch and spread the virus. The trend also doesn't imply that the virus spreads exclusively through sexual activity. Sex raises the risk of mpox transmission due to the skin-to-skin contact and prolonged face-to-face contact typically involved, but the virus also spreads through nonsexual close contact.
Infectious diseases tend to ripple through social networks because, in many cases, they rely on human interaction to spread. As of now, men who have sex with men have been the hardest hit by the outbreak, but experts at the WHO expect that trend to change over time, CNN reported.
This article is for informational purposes only, and is not meant to offer medical advice.
Originally published on Live Science.

Nicoletta Lanese is the health channel editor at Live Science and was previously a news editor and staff writer at the site. She holds a graduate certificate in science communication from UC Santa Cruz and degrees in neuroscience and dance from the University of Florida. Her work has appeared in The Scientist, Science News, the Mercury News, Mongabay and Stanford Medicine Magazine, among other outlets. Based in NYC, she also remains heavily involved in dance and performs in local choreographers' work.
 Live Science Plus
Live Science Plus