HIV/AIDS: Facts about the viral infection that attacks the immune system
Learn how HIV spreads, how it affects the body and what treatments are available.
Get the world’s most fascinating discoveries delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?
Join the club
Get full access to premium articles, exclusive features and a growing list of member rewards.
What it is: A lifelong viral infection that weakens the immune system, if left untreated
Prevention methods: Taking preventive medicines called PrEP, using condoms, and avoiding needle sharing
Treatments: Medicines called antiretroviral therapy (ART)
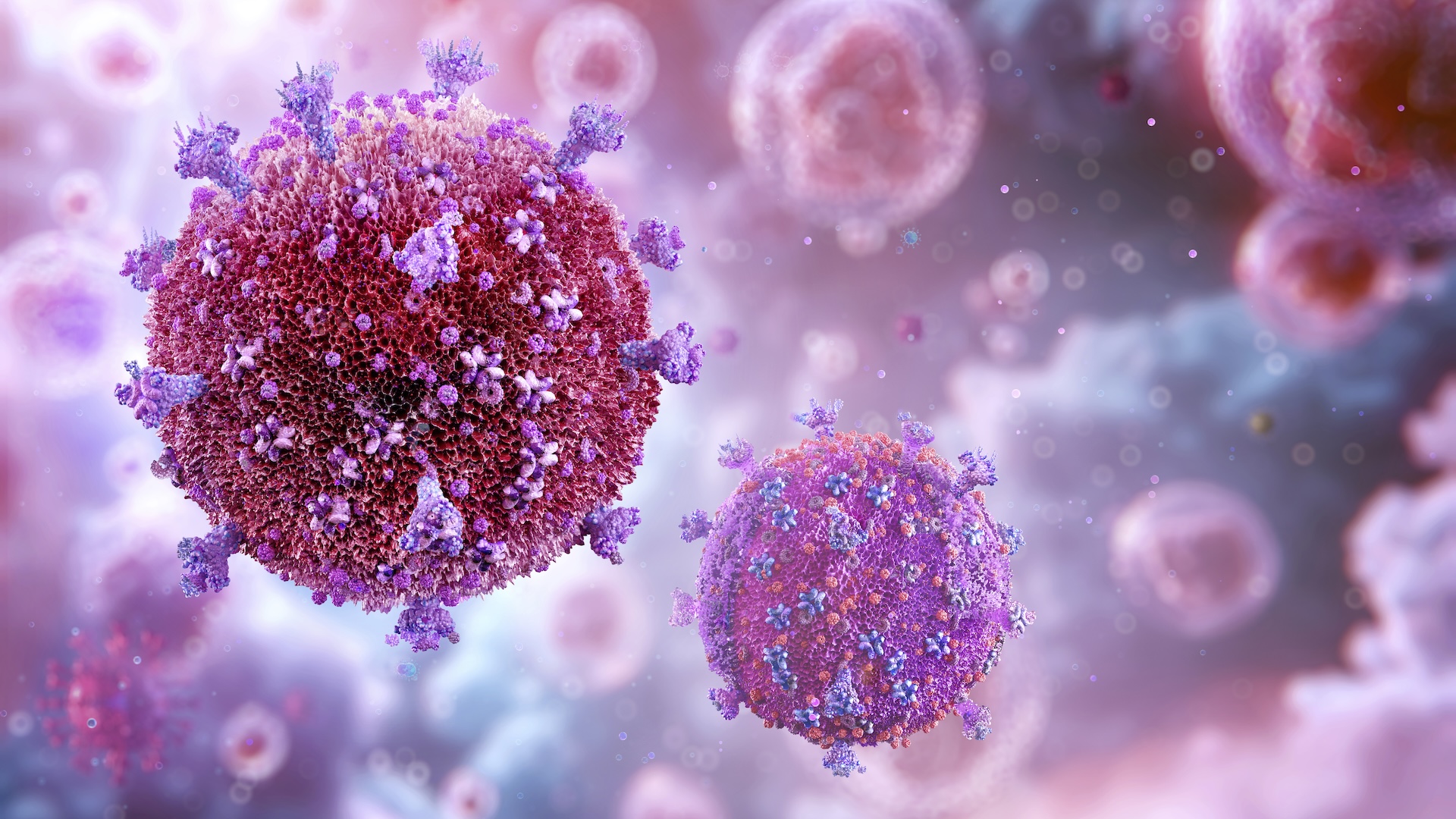
Human immunodeficiency virus (HIV) is a germ that causes a lifelong infection that slowly weakens the immune system. Though the infection is lifelong, medicines can keep the virus in check and help people reach lifespans of near-normal length.
However, when people don't have access to those medicines, HIV infections progress to an advanced stage called acquired immunodeficiency syndrome (AIDS), which is fatal within about three years if not treated. When a person has AIDS, most of their key, disease-fighting immune cells are lost. This loss of immune protection leaves the person vulnerable to deadly infections and cancers.
Although an HIV diagnosis was once a death sentence, scientists have developed treatments that suppress the virus and enable people to live long lives without transmitting the disease to others. Additionally, there are now effective preventive medications that can dramatically reduce the risk of getting HIV in the first place.
There is not yet a widespread cure for HIV/AIDS, although a handful of people have been cured of the infection or are in long-term remission thanks to special stem-cell transplants, specially cell transplants from people who have genes that make them resistant to the virus. Scientists are exploring potential avenues for a cure, which could someday mean that people who contract HIV could be rid of the infection rather than having to take medication for life to manage the disease.
HIV/AIDS remains a major public health threat worldwide, with an estimated 39.9 million people living with the disease at the end of 2023. Around 630,000 people died from illnesses related to AIDS the same year; by weakening the immune system, AIDS opens the door to these fatal diseases.
Everything you need to know about HIV
How does HIV spread?
HIV can spread through contact with an infected person's bodily fluids, although it's important to note that not all bodily fluids can transmit the virus.
Bodily fluids that can spread HIV include blood, semen, preseminal fluid, vaginal secretions, breastmilk and rectal discharge (liquid from the anus that's not blood or stool). HIV is not transmitted through saliva, sweat or tears. It's also not spread through the air or through casual contact, such as hugging, shaking hands or sharing food.
For transmission to occur, the bodily fluids containing HIV must come into contact with mucous membranes — tissues that line cavities in the body, like the vagina, anus or mouth. The fluids can also transmit HIV when they come into contact with cuts or sores, or when they're introduced to the bloodstream via contaminated needles, for instance.
Most people who contract HIV get it through unprotected anal or vaginal sex — meaning sex without a condom or without HIV-preventing medications. People can also contract the virus by sharing the equipment used to inject drugs, such as needles or syringes.
Babies can get HIV in the womb, during childbirth or from breastfeeding, if their mother has HIV.
People living with HIV who take medicines called ART can suppress the virus to the point that it can't spread via sex. These "virally suppressed" people also have a much lower chance of transmitting HIV to their kids via pregnancy, childbirth or breastfeeding. They are also less likely to spread the virus via shared injection equipment, although experts aren't sure exactly how much the risk is reduced.
What are the symptoms of HIV/AIDS?
The symptoms of HIV vary depending on how far the disease has progressed. The virus can spread from one person to another at any stage of the infection, unless the infected person is taking ART and has reached "viral suppression" (see glossary).
The initial stage is called "acute HIV infection." Within two to four weeks of contracting the virus, many people develop a flu-like illness involving symptoms like fever, headache, rash and sore throat. These symptoms can last from a few days to a few weeks. Some people have no symptoms at this stage, however. The viral load, or amount of HIV in the blood, at this stage is very high.
The second stage of the disease is "chronic HIV infection," during which the virus continues to multiply but at a slower speed than during acute infection. This stage is also called "clinical latency" or "asymptomatic HIV infection," as many people don't feel sick during it. People can remain in this stage of the disease for 10 to 15 years, though some pass through it more quickly.
As the virus multiplies, levels of an important type of immune cell — CD4 T lymphocytes — decline. Without treatment, the disease will eventually enter its most advanced stage: AIDS. This can come with a wide range of symptoms, including rapid weight loss; recurring fever; night sweats; extreme tiredness; prolonged swelling of the lymph nodes; diarrhea; sores of the mouth, anus or genitals; and blotches on or under the skin or inside the mouth, nose or eyelids. It can also trigger neurological problems, like memory loss.
AIDS raises the risk of severe bacterial infections and cancers, including lymphomas and Kaposi's sarcoma. It can also worsen viral infections, such as hepatitis B and mpox. Without any treatment, people with AIDS typically survive about three years.
What is the difference between HIV and AIDS?
HIV and AIDS are related, in that AIDS is the most advanced stage of an HIV infection, and therefore, the HIV virus causes both conditions. AIDS can also be called a "stage 3 HIV infection."
AIDS is defined in part by a very low CD4 count of fewer than 200 CD4 cells per cubic millimeter (mm3) of blood. Generally speaking, the CD4 counts of healthy teens and adults are around 500 to 1,200 cells/mm3. Anything below 500 cells/mm3 is considered low, and 200 cells/mm3 marks the threshold for an AIDS diagnosis.
Doctors also diagnose AIDS by considering a patient's history of "AIDS-defining illnesses." These are medical conditions often seen in people with AIDS because their immune systems can't fight the illnesses off. They include "opportunistic" infections — those caused by germs that wouldn't necessarily harm a person with a well-functioning immune system.
Such infections include a fungal infection called extrapulmonary cryptococcosis, recurrent blood infections with Salmonella bacteria, the parasitic infection toxoplasmosis, and lower respiratory infections caused by the herpes simplex virus. The bacterial disease tuberculosis poses a major risk to people with AIDS, and it is currently the leading cause of death for people living with HIV/AIDS worldwide.
AIDS-defining illnesses also include cancers such as Kaposi's sarcoma, Burkitt's lymphoma and invasive cervical cancer. Others include HIV encephalopathy, which affects brain function, and HIV wasting syndrome, which causes extreme weight loss and weakness. Complications of AIDS-defining illnesses raise the risk of death, but the degree of risk varies among diseases.
How is HIV treated?
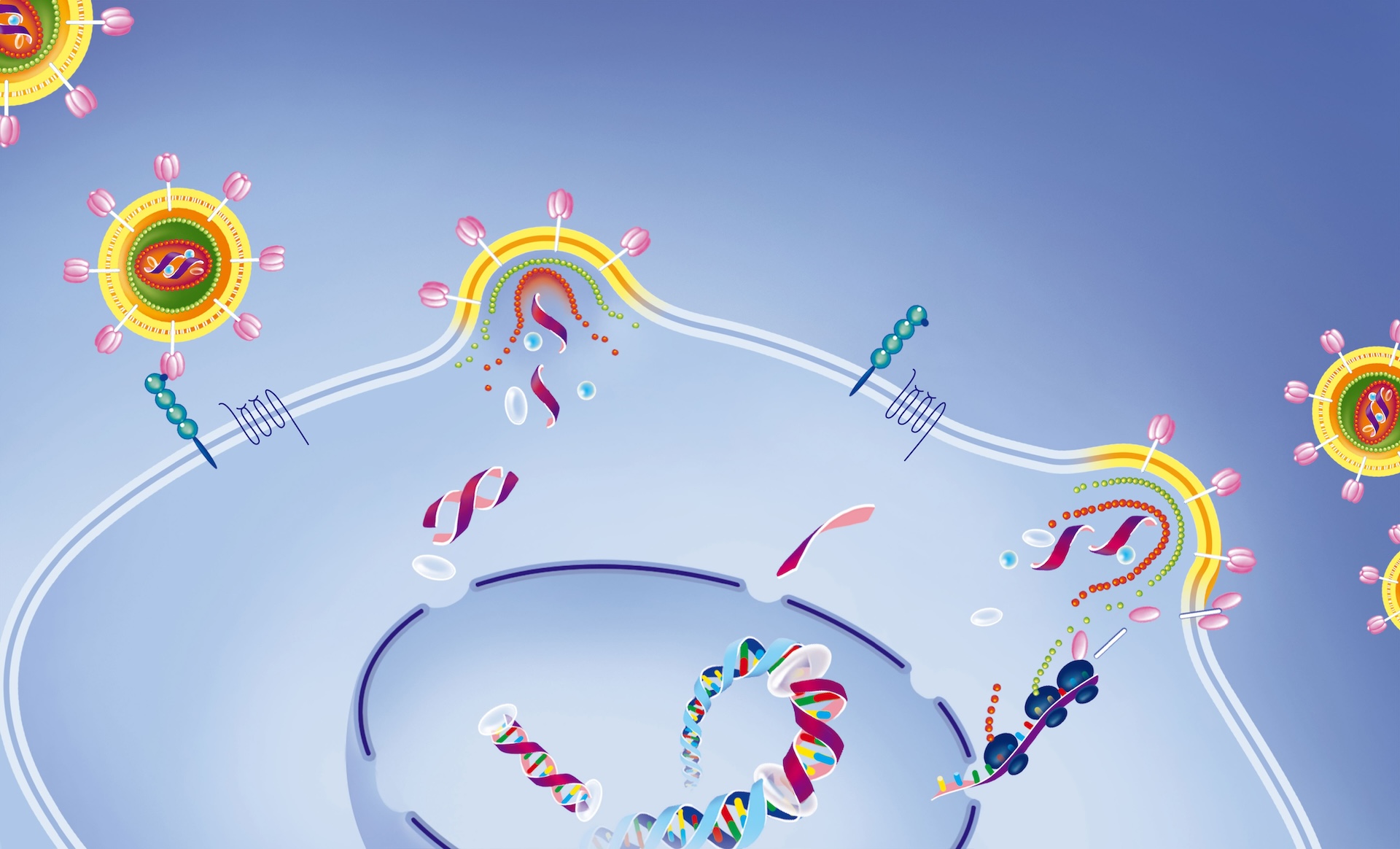
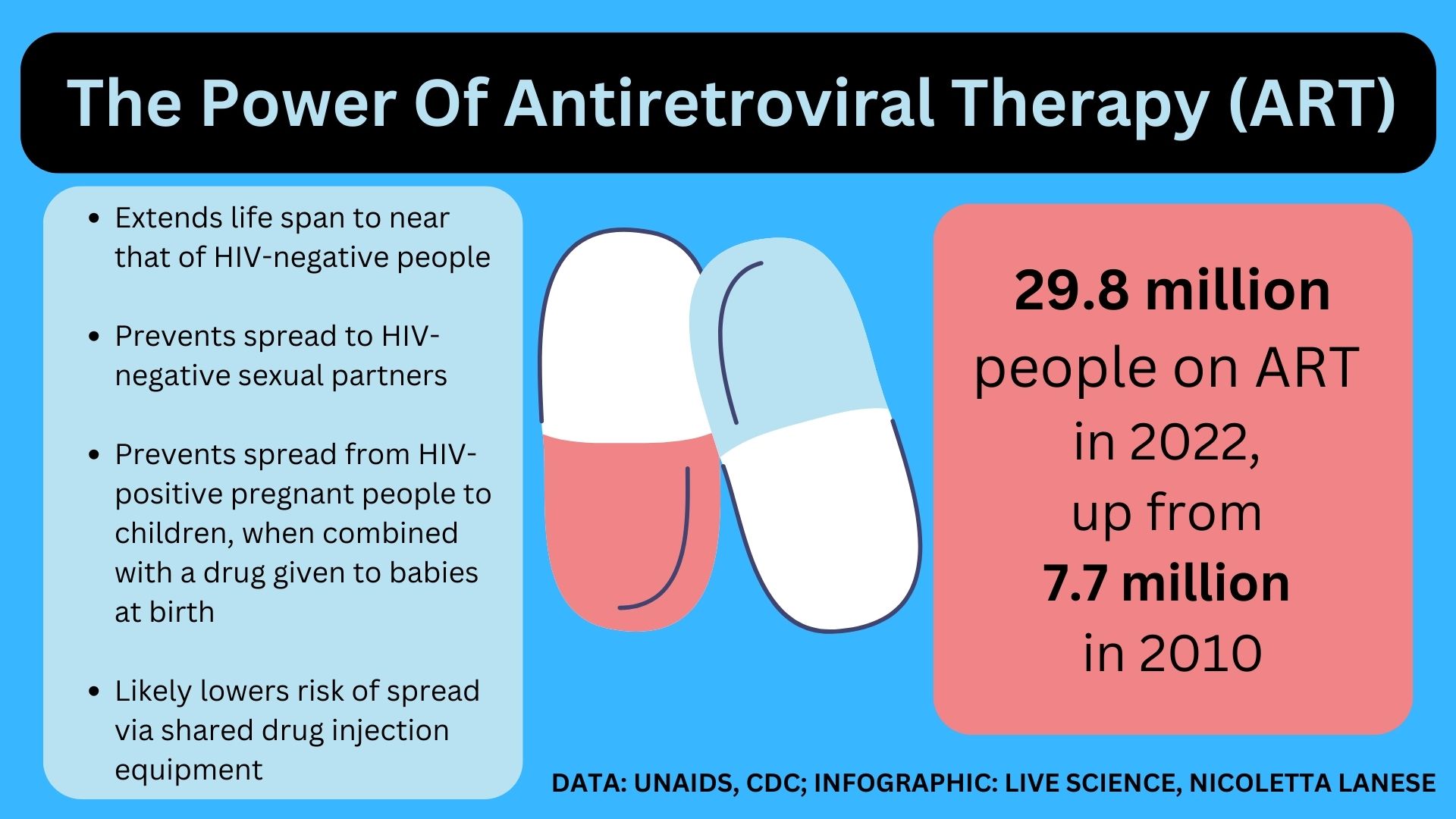
At all three stages of the infection, HIV is treated with antiretroviral therapy (ART) — combinations of medications that drive down the amount of HIV in the blood. Different ART drugs work in different ways to keep the amount of virus, or viral load, in check. They are available as daily pills or as shots given periodically throughout the year, depending on the person's treatment plan.
It's key for patients to take their medication as prescribed, because missing pills or shots can open the door for the virus to multiply, as well as develop drug resistance, which causes the medication to work less well. ART medications can also interact with other drugs and carry some risk of serious side effects, so patients work with their medical providers to figure out which drug combination is best for them.
The goal of ART is "viral suppression," which describes when a person's viral load falls low enough that there are 200 or fewer copies of the virus's genetic material per milliliter (mL) of blood. Historically, tests weren't sensitive enough to detect levels of HIV below that threshold, so doctors called this level "undetectable."
Studies also found that people who reach viral suppression can't transmit the virus via sex; have a lower chance of spreading the virus through pregnancy, childbirth or breastfeeding; and likely have a lower chance of spreading it through needle sharing. This is why the slogan "undetectable equals untransmittable," or "U = U," was coined.
Nowadays, some tests for HIV are extremely sensitive, so they can detect viral loads significantly below 200 copies/mL. However, experts emphasize that 200 copies/mL is still the critical threshold at which transmission risk becomes extremely low.
If a person with HIV/AIDS develops another medical condition, such as an AIDS-defining illness, the individual would receive treatment for that condition in addition to their ART regimen.
Can HIV/AIDS be cured?
There is no widespread cure for HIV/AIDS. However, a handful of people have been cured of their HIV infections through stem cell transplants, and a few more are considered "potentially" cured via the same process.
Stem cells can develop into different types of cells in the body. In certain cancers that affect blood cells, stem cell transplants can be used to replace the cells lost in the course of cancer treatments such as chemotherapy. Each individual who has been cured of HIV also had one of these cancers, so their doctors searched for stem cell donors who carry a rare gene that makes them resistant to HIV infection. By swapping in cells from an HIV-resistant individual, the procedure essentially locks the virus out of the patient's CD4 cells.
There is one exception to this rule: A person known as the "Geneva patient" was potentially cured of HIV after a stem cell transplant, but the donor didn't have this special genetic resistance. It's unclear exactly why the man entered long-term remission from the infection after this procedure, but scientists are investigating.
There have also been a couple of cases in which people's own immune systems somehow rallied against the virus and controlled it without treatment; these people are known as "elite controllers."
Scientists hope to learn from both the stem cell recipients and from elite controllers to discover cures that could reach far more people with HIV/AIDS. Meanwhile, some researchers are exploring the use of gene-editing tools like CRISPR to cure the infection, while others are investigating the use of drugs and modified immune cells.
Glossary
- Antiretroviral therapy (ART) – Combinations of medications that lower the amount of HIV in a person's blood. These drugs, given as pills or shots, prevent the viral infection from progressing to AIDS and dramatically lower a person's risk of complications and of transmitting the virus to others.
- Pre-exposure prophylaxis (PrEP) – Medicines that people at risk of being exposed to HIV take to prevent the infection.
- Viral load – The amount of HIV in a person's blood. This is measured in terms of the number of HIV RNA molecules — the virus's genetic material — found in a milliliter of blood. It's an important way to measure how well ART is working.
- Viral suppression – When a person's viral load falls to 200 copies/mL or lower. Viral suppression is the goal of ART, as it both lowers a person's likelihood of spreading the virus and extends their lifespan by preventing the infection from progressing to AIDS.
- CD4 T lymphocyte – A type of white blood cell that helps coordinate the actions of other immune cells to fight infections. HIV infects CD4 cells and uses them to multiply while the virus depletes the number of CD4 cells in the body.
HIV/AIDS pictures

ACT UP
In the 1980s and 1990s, groups organized "die-ins" to protest the lack of U.S. government attention to the ongoing HIV/AIDS crisis. Die-ins were also conducted to push for support for research to uncover effective treatments and, once treatments were discovered, to demand that those drugs be released to the public. The AIDS Coalition to Unleash Power — known as ACT UP — was a major force behind such protests and remains an active organization today.

Kaposi's sarcoma
Kaposi's sarcoma, an example of an AIDS-defining illness, characteristically causes big, purple patches or nodules to appear on the skin and mucous membranes.

U = U
The public health slogan "U = U," depicted on this sign, refers to the fact that people living with HIV who have undetectable viral loads cannot transmit the virus to others via sex. It stands for "undetectable = untransmittable."

The "Berlin patient"
The "Berlin patient," pictured here, was the first person cured of HIV via a stem cell transplant. His name was later revealed to be Timothy Ray Brown. Brown went on to launch a foundation under his name that was dedicated to fighting HIV/AIDS.
Discover more about HIV
- We could end the AIDS epidemic in less than a decade. Here's how.
- In a 1st, HIV vaccine triggers rare and elusive antibodies in humans
- Nearly 3 million extra deaths by 2030 could result from HIV funding cuts, study suggests
Get the world’s most fascinating discoveries delivered straight to your inbox.

Nicoletta Lanese is the health channel editor at Live Science and was previously a news editor and staff writer at the site. She holds a graduate certificate in science communication from UC Santa Cruz and degrees in neuroscience and dance from the University of Florida. Her work has appeared in The Scientist, Science News, the Mercury News, Mongabay and Stanford Medicine Magazine, among other outlets. Based in NYC, she also remains heavily involved in dance and performs in local choreographers' work.
You must confirm your public display name before commenting
Please logout and then login again, you will then be prompted to enter your display name.
 Live Science Plus
Live Science Plus










