Reproductive System: Facts, Functions & Diseases
The reproductive system is a collection of internal and external organs — in both males and females — that work together for the purpose of procreating, according to the Cleveland Clinic. Due to its vital role in the survival of the species, many scientists argue that the reproductive system is among the most important systems in the entire body.
How reproductive systems work
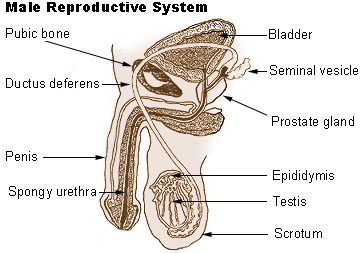
The male reproductive system consists of two major parts: the testes, where sperm are produced, and the penis, according to Merck Manuals. The penis and urethra belong to both the urinary and reproductive systems in males. The testes are carried in an external pouch known as the scrotum, where they normally remain slightly cooler than body temperature to facilitate sperm production.
- Related: Probiotics for vaginal health
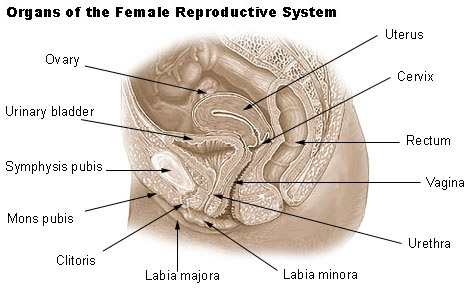
The external structures of the female reproductive system include the clitoris, labia minora, labia majora and Bartholin's glands, according to the Cleveland Clinic. The major internal organs of the female reproductive system include the vagina and uterus — which act as the receptacle for semen — and the ovaries, which produce the female's ova. The vagina is attached to the uterus through the cervix, while the fallopian tubes connect the uterus to the ovaries. In response to hormonal changes, one ovum, or egg — or more in the case of multiple births — is released and sent down the fallopian tube during ovulation. If not fertilized, this egg is eliminated during menstruation.
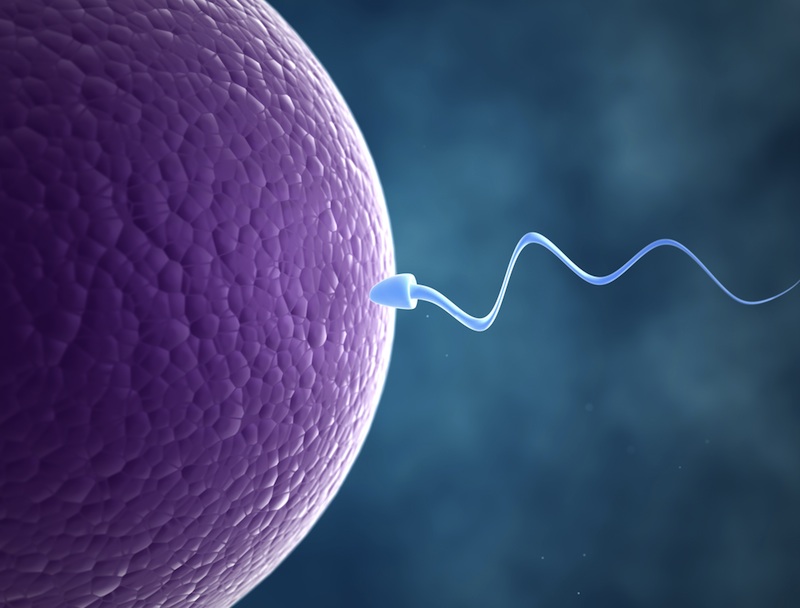
Fertilization occurs if a sperm enters the fallopian tube and burrows into the egg. While the fertilization usually occurs in the oviducts, it can also happen in the uterus itself. The egg then becomes implanted in the lining of the uterus, where it begins the processes of embryogenesis (in which the embryo forms) and morphogenesis (in which the fetus begins to take shape). When the fetus is mature enough to survive outside of the womb, the cervix dilates, and contractions of the uterus propel it through the birth canal.
Variations in the reproductive system
Around 49.5 percent of the world's population is female, so there are slightly more men on the planet than women, according to World Bank. A person's sex is determined by what reproductive system the person has, but it isn't always so simple. Some humans are born with parts of both male and female reproductive systems or incomplete reproductive organs of one sex or the other. Those with both male and female reproductive parts are considered intersex. Sometimes children are labeled as male or female, depending on how complete or functional one sexual reproductive system is over the other. Then, the other organs are removed.
Today, many parents are opting to leave both sets of reproductive organs intact with the intent of letting the child decide to keep or remove the various parts when they are older. A baby is born atypical genitalia in one in about 1,500 to 2,000 births, according to Intersex Society of North America.
Females that are born without all of their reproductive system are labeled as having Mayer Rokitansky Kuster Hauser Syndrome. This occurs in one in 5,000 female births, according to the Center for Young Women’s Health.
Get the world’s most fascinating discoveries delivered straight to your inbox.
Diseases of the female reproductive system
Many parts of the male and female reproductive systems can be affected by cancer. In females, cancer can attack the uterus, ovaries, breast and cervix, among other organs, according to the American Cancer Society.
Many experts have seen what they refer to as the "Angelina Jolie" effect, where women are taking proactive measures by having breasts and internal reproductive organs removed if they have a family history of cancer before there are signs of the disease. "With better genetic testing and screening, we have seen a number of women who are being more proactive about their reproductive health," said Dr. Shana Wingo, who specializes on gynecologic oncology at Arizona Oncology.
Ovarian cancer tends to have a poorer outcome than other gynecological cancers, Ross noted, because it is not typically diagnosed until it has progressed significantly. "There is no standard screening available for ovarian cancer, so it is very difficult to identify it early."
Tests to detect ovarian cancer, as well as cancer of the fallopian tube, and primary peritoneal cancer are currently being studied, according to the National Cancer Institute.
There are two tests used to screen for cervical cancer. The Pap test screens for cellular changes in the cervix called cytology, while the genital human papillomavirus (HPV) test identifies the presence of infection with high-risk HPV, the strains that are linked to cervical cancer, according to Dr. Charles Dubin, an OB/GYN in Santa Monica, Calif.
A recent study published by Cancer Cytopathology, found that HPV-only screening misses more cervical cancer in women than Pap-only or co-testing, based on approximately 8.6 million women ages 30 to 65. There is approximately a three-fold improvement in the cancer detection rate of co-testing compared to HPV only.
Current guidelines recommend that women first start getting the Pap test alone when they turn 21 and repeat every three years if the test is normal until age 30. A Pap-plus-HPV test, or co-testing, is recommended for women ages 30 to 65, and if both are negative repeated every five years, regardless of whether they have received HPV vaccination. "However, there is compelling scientific evidence that co-testing every three years misses less cases of cancer and pre-cancer than every five-year co-testing," Dubin noted.
While genital HPV is typically associated with females, it is the most common sexually transmitted infection. The majority of sexually active people in the United States — male and female — will have HPV at some time in their lives, but most will not experience any symptoms. In a small portion of women, it can result in cervical cancer and genital warts; in men, it can cause penile and anal cancer and genital warts, according to the NIH.
Both genders can develop sexually transmitted diseases, including genital herpes, gonorrhea and syphilis, according to the National Institutes of Health (NIH). HIV/AIDS, a disease of the immune system, is not exclusively transmitted through sexual contact; sexual activity is one of the ways that the HIV virus is spread.
For females, severe menstrual cramping, or dysmenorrheal, is the most common disease of the reproductive system occurs with a woman's monthly menstrual period, according to Dr. Sheryl Ross, OB/GYN and Women's Health Specialist at Providence Saint John’s Health Center.
"Severe pain before or during your period can last anywhere from one to seven days and disrupt your normal day-to-day routines at school, work and socially," Ross noted. Diagnosis is made by the patient's medical history and a pelvic exam. The best treatment includes medications that block the effects of prostaglandins and include ibuprofen and naproxen. The birth control pill also works well in treating dysmenorrhea by decreasing the blood flow, Ross noted.
Another common disorder of the female reproductive system is a vaginal yeast infection, which is caused by a yeast fungus in the vagina. Most can be successfully treated with over-the-counter medications, according to WebMD.
Endometriosis is a condition where that normally lines the inside of your uterus — the endometrium — ends up outside of uterus, most commonly in the ovaries, bowel or the tissue lining your pelvis. The endometrial tissue becomes trapped, causing pain, according to the Mayo Clinic.
Pelvic inflammatory disease can involve an infection of any of the female reproductive organs, including the uterus and ovaries. Sexually transmitted diseases, such as gonorrhea and chlamydia, are typical causes of pelvic inflammatory disease, according to the NIH. "Any of these STIs can cause serious and potentially long term reproductive problems that include chronic pelvic pain and infertility," Ross said.
Diseases of the male reproductive system
Of male-specific diseases of the reproductive system, prostate cancer is the most common, but men can also suffer from testicular and penile cancer, according to the American Cancer Society.
Treatment for prostate cancer depends on the age, severity of the disease and other health conditions of the patient. The usual treatments for prostate cancer are surgery, radiation therapy, watchful waiting, and hormonal treatment, according to the Cleveland Clinic.
Erectile dysfunction is a common condition that affects about one in 10 males on a long-term basis, the Cleveland Clinic noted. It can be linked to vascular disease, neurological disorders such as Multiple Sclerosis, trauma and psychological episodes.
Prostatitis typically involves swelling or inflammation of the prostate gland, according to the Mayo Clinic, and can cause painful or difficult urination and ejaculation. Nearly half of all men experience symptoms of prostatitis at some point during their lives.
Defining and treating infertility
Infertility is defined as a couple's inability to conceive after one year of unprotected intercourse. It can be caused by a condition in one partner or a combination of circumstances, according to the Mayo Clinic.
In males, infertility is a condition in which they produce no sperm cells (azoospermia) or too few sperm cells (oligospermia), or their sperm cells are abnormal or die before they can reach the egg. Causes range from chromosomal defects to hormonal imbalance to tumors. Lifestyle factors, such as drug and alcohol use, can also play role. In rare cases, infertility in men is caused by an inherited condition, such as cystic fibrosis, according to the Mayo Clinic.
In women, infertility is defined as a disorder of the reproductive system that hinders the body's ability to ovulate, conceive, or carry an infant to term.
Reproductive conditions are treated by a variety of specialists. In women, many issues are treated by obstetricians/gynecologists and for males, urologists handle many disorders of their reproductive systems. There are also infertility experts that treat couples who are unable to conceive and endocrinologists who treat hormonal disorders.
Additional reporting by Alina Bradford, Live Science contributor.
Editor’s Note: If you’d like more information on this topic, we recommend the following book:
Systems of the human body
- Circulatory System: Facts, Function & Diseases
- Digestive System: Facts, Function & Diseases
- Endocrine System: Facts, Functions and Diseases
- Immune System: Diseases, Disorders & Function
- Lymphatic System: Facts, Functions & Diseases
- Muscular System: Facts, Functions & Diseases
- Nervous System: Facts, Function & Diseases
- Respiratory System: Facts, Function & Diseases
- Skeletal System: Facts, Function & Diseases
- Skin: Facts, Diseases & Conditions
- Urinary System: Facts, Functions & Diseases
Parts of the human body
- Bladder: Facts, Function & Disease
- Human Brain: Facts, Anatomy & Mapping Project
- Colon (Large Intestine): Facts, Function & Diseases
- Ears: Facts, Function & Disease
- Esophagus: Facts, Function & Diseases
- How the Human Eye Works
- Gallbladder: Function, Problems & Healthy Diet
- Human Heart: Anatomy, Function & Facts
- Kidneys: Facts, Function & Diseases
- Liver: Function, Failure & Disease
- Lungs: Facts, Function & Diseases
- Nose: Facts, Function & Diseases
- Pancreas: Function, Location & Diseases
- Small Intestine: Function, Length & Problems
- Spleen: Function, Location & Problems
- Stomach: Facts, Function & Diseases
- The Tongue: Facts, Function & Diseases
Additional resources
- NIH: Aging changes in female reproductive system, and in male reproductive system
- CDC: Women's Reproductive Health & Men's Reproductive Health
Kim Ann Zimmermann is a contributor to Live Science and sister site Space.com, writing mainly evergreen reference articles that provide background on myriad scientific topics, from astronauts to climate, and from culture to medicine. Her work can also be found in Business News Daily and KM World. She holds a bachelor’s degree in communications from Glassboro State College (now known as Rowan University) in New Jersey.