Printable Skin: 'Inkjet' Breakthrough Makes Human Tissue
By manufacturing human skin cells using a printer similar to an inkjet, scientists have taken a significant first step toward generating new skin. The process, which could revolutionize the treatment of major skin wounds, could be ready for clinical trials in five years.
While much research needs to be done, the technique is promising, according to an expert not involved in the breakthrough.
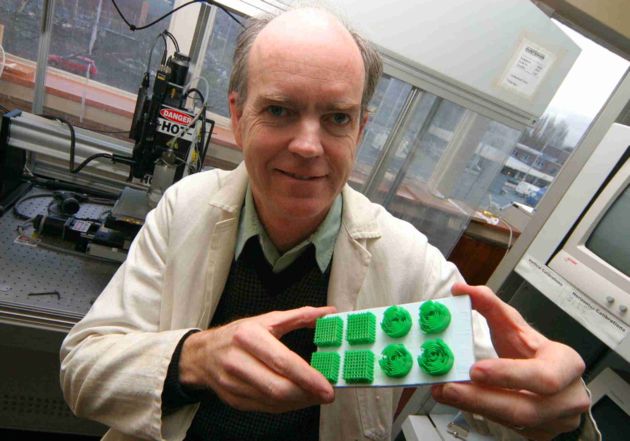
Scientists expect to eventually build commercial skin printers for hospital use. Doctors would take cells from a patient's body, multiply them, and suspend them in a nutrient-rich liquid similar to ink. A technician would enter measurements of a patient's wound into a computer and feed the suspended cells into the printer.
The cells would then be seeded on a plastic tissue scaffold, which provides shape and stability to the new piece of skin as it develops. The scaffold would also anchor the perfectly shaped piece of skin over the wound, once applied, keeping the graft in place until it takes hold.
The scaffold would dissolve naturally over time, just as some stitches do.
"The cells are the patient's own cells and the object is to reincorporate them into the body," project leader Brian Derby told LiveScience.
Perhaps bones and organs, too
Get the world’s most fascinating discoveries delivered straight to your inbox.
Derby heads the Ink-Jet Printing of Human Cells Project at the University of Manchester in the United Kingdom. He said that using a person's own cells is ideal because it will reduce scarring, and patients will not need to take immunosuppressant drugs, as they do with some current skin transplant procedures.
Derby's team is using starter cells taken from patients having hip implants at the Manchester Royal Infirmary, but the ideal situation would be to take stem cells from a patient's bone marrow and control how they morph, a natural process called differentiation. Stem cells can become any type of body tissue when properly directed.
The technology would allow printing more than one type of cell at a time and, overcoming a current limitation, allow control over the shape of whatever is grown. The shape of the scaffold determines the shape of the end product.
"It would be possible to build up a structure using different cell types mimicking the structure of actual skin," Derby said. "You can print as many cells as you have print heads. Our machine could print up to eight different 'inks' where the inks are cell suspensions, scaffold materials or biochemicals."
Such a printer could possibly generate bone for bone grafts, or even whole organs, although these goals are farther down the research road.
"In theory, you could print the scaffolding to create an organ in a day, but we are not quite there yet," Derby said.
'Significant achievement'
Ioannis Yannas, a professor at Massachusetts Institute of Technology, is the co-developer of the Dermis Regeneration Template (DRT), the first "artificial skin" scaffold developed. It was given federal approval in 1991 for use in plastic surgery and in 1996 to treat burns. DRT has been used with more than 13,000 burn victims.
Derby's research is a "significant achievement," Yannas said in an email interview. "Dr. Derby's process promises to greatly simplify cell-seeding of scaffolds that are used to induce organ regeneration."
It's not yet clear, however, whether the technology will go beyond production of skin.
"It remains to be seen whether the process can be used to seed scaffolds that have been shown capable of inducing regeneration leading to restoration of organ shape and physiological function," Yannas said.
Yannas' DRT process involves a mesh consisting mostly of collagen fibers that is placed on a wound to provide a structure for new dermis (sub-layer of skin) and its structures to grow on. Once that is complete, a very thin layer of epidermis (top-layer of skin) is harvested from the patient's body and is placed over the new dermis. The DRT prevents contraction and scar formation, and helps the body grow new, pliable skin, typically in 30 days.
Teams in the United States and Japan are also working on systems similar to the new inkjet technology, but Derby's team is the first to produce cells without destroying them during the printing process. The scaffolds are very small -- on the scale of millimeters, but Derby expects to create 3D scaffolds on the scale of centimeters by November. A centimeter is 0.4 inches.
Derby hopes to move to clinical trials soon. "There is a fighting chance something could come of this in five years," he said.
 Live Science Plus
Live Science Plus