Scientists created human egg cells from skin cells — then used them to make embryos
In a proof-of-concept experiment, scientists demonstrated that you can create and fertilize human eggs in the lab using sperm, genes from skin cells, and the "shells" of existing egg cells.

Get the world’s most fascinating discoveries delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?

Delivered Daily
Daily Newsletter
Sign up for the latest discoveries, groundbreaking research and fascinating breakthroughs that impact you and the wider world direct to your inbox.

Once a week
Life's Little Mysteries
Feed your curiosity with an exclusive mystery every week, solved with science and delivered direct to your inbox before it's seen anywhere else.

Once a week
How It Works
Sign up to our free science & technology newsletter for your weekly fix of fascinating articles, quick quizzes, amazing images, and more

Delivered daily
Space.com Newsletter
Breaking space news, the latest updates on rocket launches, skywatching events and more!

Once a month
Watch This Space
Sign up to our monthly entertainment newsletter to keep up with all our coverage of the latest sci-fi and space movies, tv shows, games and books.

Once a week
Night Sky This Week
Discover this week's must-see night sky events, moon phases, and stunning astrophotos. Sign up for our skywatching newsletter and explore the universe with us!
Join the club
Get full access to premium articles, exclusive features and a growing list of member rewards.
Scientists have created human eggs in the lab using a similar process to the one used to clone the famous Dolly the sheep, then used in vitro fertilization (IVF) to turn them into embryos.
Although this method is far from being used in a clinical setting, the hope is that it could eventually pave the way to new fertility treatments.
"In addition to offering hope for millions of people with infertility due to lack of eggs or sperm, this method would allow for the possibility of same-sex couples to have a child genetically related to both partners," study co-author Dr. Paula Amato, a professor of obstetrics and gynecology in the Oregon Health & Science University (OHSU) School of Medicine, said in a statement.
The proof-of-concept experiment was described Tuesday (Sept. 30) in the journal Nature Communications.
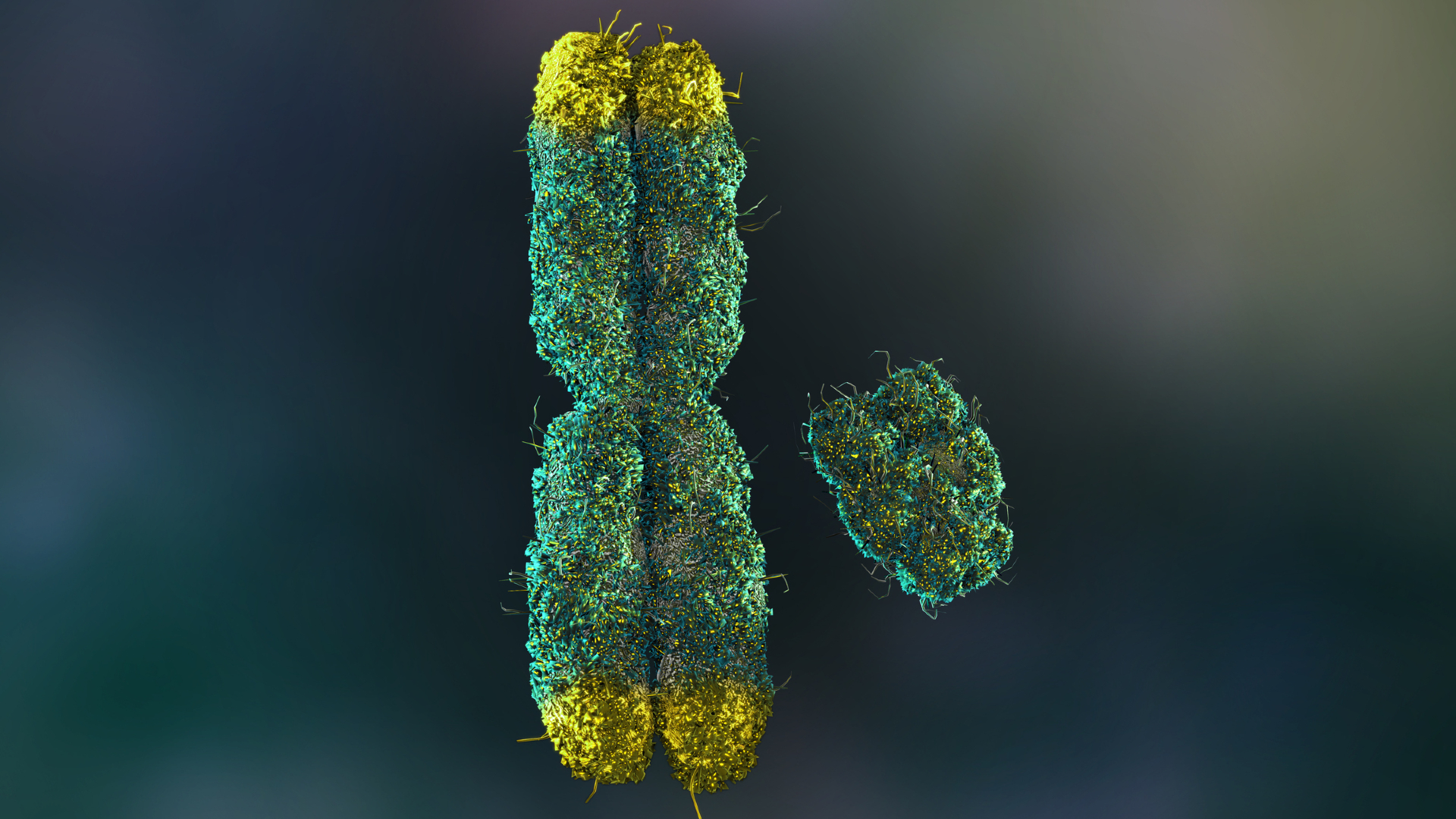
The egg-making process involved removing the nucleus from an existing human egg cell and swapping it out for a nucleus from a human skin cell. This first step, called somatic cell nuclear transfer, has been used to clone a variety of animals, including Dolly.
But the OHSU researchers aimed to make a functional egg, not a clone, and eggs carry half the chromosomes as nonreproductive cells in the body do. During fertilization, an egg's 23 chromosomes combine with 23 chromosomes from a sperm cell, resulting in a total of 46. To prompt their makeshift eggs to shed half their chromosomes, the scientists applied an electrical pulse and a drug called roscovitine, which messes with enzymes that regulate the cell cycle, the process by which cells divide.
This experiment ultimately resulted in 82 egg cells that were then fertilized with sperm via in vitro fertilization (IVF), according to the statement. However, the fertilization step isn't yet foolproof — only around 9% made it to the "blastocyst" stage. At that point, the egg has divided to form a hollow sphere of cells that could be introduced to the womb via IVF.
Get the world’s most fascinating discoveries delivered straight to your inbox.
Most of the eggs fertilized in the study didn't make it to the blastocyst stage, and in fact, only divided enough times to produce four to eight cells overall.
The "modest" blastocyst development rate likely stems from two factors, the study authors wrote in their paper. For starters, chromosomal abnormalities likely stopped the fertilized eggs from dividing further. And second, the genes swapped in from skin cells likely weren't successfully reprogrammed to sustain embryonic development. In other words, in some ways, the genes were still activating as if they were in skin cells, not the cells that form early in development.
It's unclear which issue presented the bigger problem in this study, but it's likely both factors contributed, the authors wrote.
None of the eggs that made it to the blastocyst stage were grown any further, and because they too bore chromosomal abnormalities, it's unlikely they would have been suitable for use in IVF, the researchers noted. These abnormalities included having too many or too few chromosomes, although on average they ended up with 46. Some eggs also carried multiple copies of the same chromosome or were missing certain chromosomes altogether.
So for now, the technique "is too inefficient and high risk to apply immediately to clinical application," Katsuhiko Hayashi, a stem cell researcher at the University of Osaka who was not involved in the study, told Science News.
The study authors also noted that "at this stage it remains just a proof of concept and further research is required to ensure efficacy and safety before future clinical applications."
Looking forward, the team plans to research how to better orchestrate the halving and then doubling of chromosomes within the egg. The goal would be to better capture what happens in a natural human pregnancy so that the right chromosomes are lost in the initial halving and then properly paired up with new chromosomes during fertilization.
If someday the technique can be refined for use in fertility treatment, however, it does raise ethical questions, experts told NPR. For instance, people could feasibly gather skin cells from others — including celebrities — without their knowledge and make functional eggs with them, Ronald Green, a bioethicist at Dartmouth College, told NPR. "It's a theoretical possibility, but not crazy," he said.
Other labs are working on different approaches to making eggs in the lab. Some have used stem cells to grow the eggs, either starting with stem cells or with adult cells that they then reverted back into stem cells. This approach has shown some success in mouse experiments but progress on the human front has been slower.

Nicoletta Lanese is the health channel editor at Live Science and was previously a news editor and staff writer at the site. She holds a graduate certificate in science communication from UC Santa Cruz and degrees in neuroscience and dance from the University of Florida. Her work has appeared in The Scientist, Science News, the Mercury News, Mongabay and Stanford Medicine Magazine, among other outlets. Based in NYC, she also remains heavily involved in dance and performs in local choreographers' work.
You must confirm your public display name before commenting
Please logout and then login again, you will then be prompted to enter your display name.
 Live Science Plus
Live Science Plus