Alzheimer's is transmissible in extremely rare scenarios
A small study suggests that "seeds" of Alzheimer's can be transferred from one person to another via certain medical procedures, leading to the disease later in life.
Get the world’s most fascinating discoveries delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?

Delivered Daily
Daily Newsletter
Sign up for the latest discoveries, groundbreaking research and fascinating breakthroughs that impact you and the wider world direct to your inbox.

Once a week
Life's Little Mysteries
Feed your curiosity with an exclusive mystery every week, solved with science and delivered direct to your inbox before it's seen anywhere else.

Once a week
How It Works
Sign up to our free science & technology newsletter for your weekly fix of fascinating articles, quick quizzes, amazing images, and more

Delivered daily
Space.com Newsletter
Breaking space news, the latest updates on rocket launches, skywatching events and more!

Once a month
Watch This Space
Sign up to our monthly entertainment newsletter to keep up with all our coverage of the latest sci-fi and space movies, tv shows, games and books.

Once a week
Night Sky This Week
Discover this week's must-see night sky events, moon phases, and stunning astrophotos. Sign up for our skywatching newsletter and explore the universe with us!
Join the club
Get full access to premium articles, exclusive features and a growing list of member rewards.
For the first time, scientists have identified people with Alzheimer's whose disease was likely triggered by a medical treatment — one that's now been banned for decades.
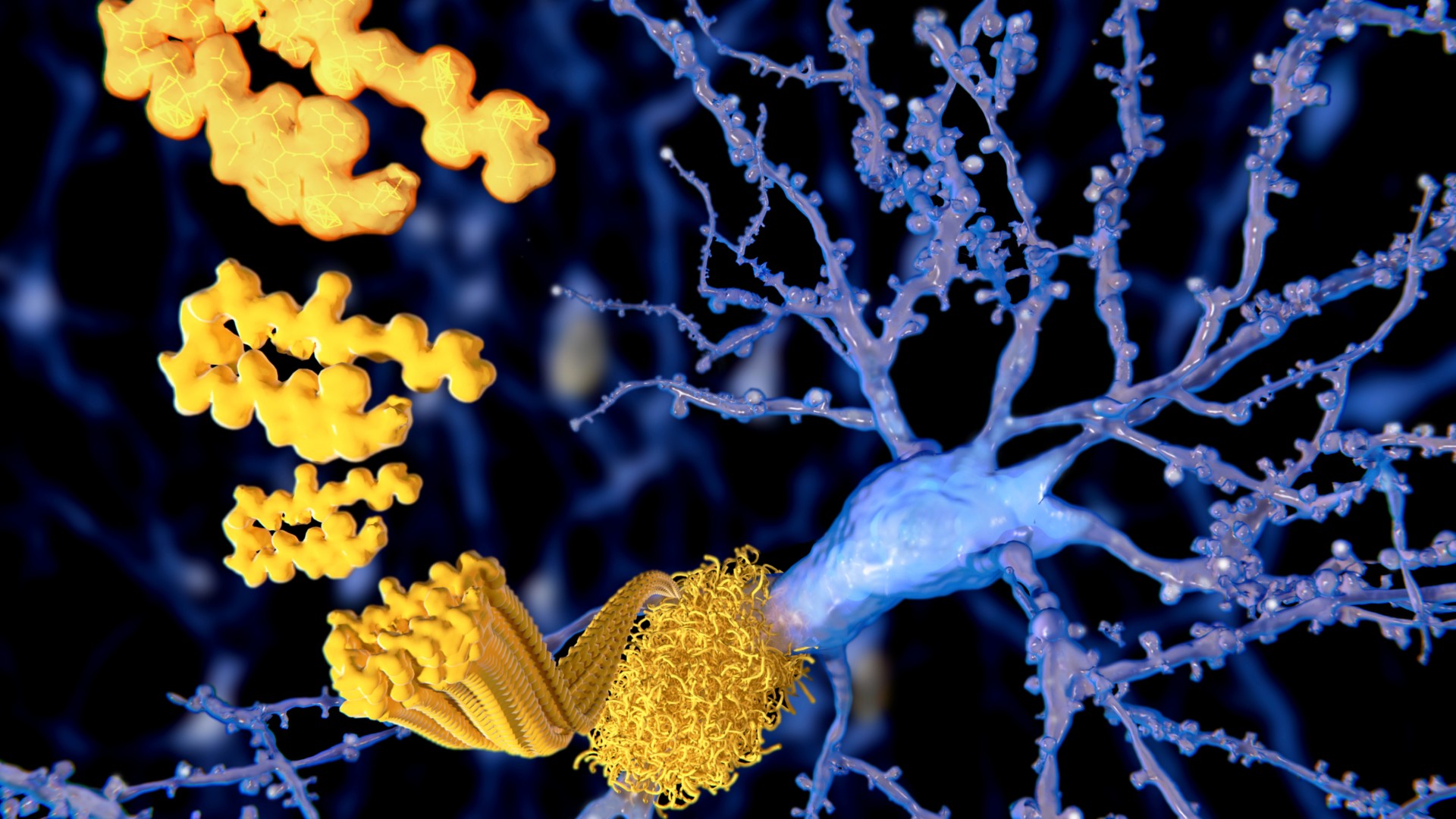
Alzheimer's is caused partly by the gradual accumulation of amyloid-beta and tau proteins in the brain, which trigger a cascade of events that lead to the death of brain cells. Now, a new study provides what may be the first clinical evidence that the "seeds" of these proteins can be extracted from one person and planted into another, sparking disease. However, this seed transfer occurred in a very specific and extraordinary medical context.
"This is not transmissible in the sense of a viral or bacterial infection," Dr. John Collinge, co-senior study author and a professor of neurology at University College London, said during a Jan. 25 news conference.
"You can't catch Alzheimer's disease by living with somebody with Alzheimer's, being a carer or a health care worker," because the "seeds" of the disease can't be transmitted that way, he emphasized.
Related: Alzheimer's comes in at least 5 distinct forms, study reveals
In the new study, published Monday (Jan. 29) in the journal Nature Medicine, researchers studied eight people in the U.K. who, as children, received a medical treatment that's now banned in many countries. Between 1959 and 1985, they received human growth hormone (hGH) that had been extracted from the brains of human cadavers.
This procedure was used to treat growth hormone deficiency — especially in the U.K., the U.S. and France — before it was banned in many countries in the 1980s. It was then replaced by synthetic versions of hGH.
Get the world’s most fascinating discoveries delivered straight to your inbox.
The cadaver-sourced hormone was ultimately banned because patients had begun dying from Creutzfeldt-Jakob disease (CJD) — a so-called prion disease that triggers an accumulation of abnormal proteins in the brain. Perhaps the most famous prion disease affects cattle and is known as "mad cow disease," or bovine spongiform encephalopathy.
Prions are proteins that act like "seeds" of disease, causing healthy proteins to fold in abnormal, harmful ways. The prions group together and form long fibers that eventually become plaques, similar to how amyloid-beta and tau propagate and grow in the brain in Alzheimer's.
In previous work, the researchers had analyzed the brains of people who died of CJD after receiving cadaver-sourced hGH. In addition to the markings of CJD, they had amyloid-beta pathology in their brains. However, because they died relatively young, it was unclear if they'd developed symptoms of Alzheimer's, or if these would have been masked by those of CJD.
Separate postmortem analyses of patients who received cadaver-sourced hGH also suggested that Alzheimer's could be spread this way, but until now, this hadn't been confirmed in living people, the authors wrote in the paper.
Related: Brain inflammation may drive mood changes in Alzheimer's
In the new study, the authors clinically assessed eight recipients of cadaver-sourced hGH who never developed CJD. Five of the eight patients had signs of early-onset dementia, with symptoms beginning between age 38 and 55. The team also analyzed proteins in the clear liquid that surrounds the patients' brains and spinal cords, and they found further evidence to support the diagnosis of Alzheimer's in two patients.
In addition, the team screened brain tissue samples from one patient who died during the study and detected signs of Alzheimer's pathology. Genetic testing ruled out the possibility that genes associated with early-onset Alzheimer's had caused any of the patients' dementia, although this data was unavailable for two of the patients.
Other variables, such as the illnesses for which the patients originally needed the hGH, may have influenced their Alzheimer's risk, the study authors noted. However, their only unifying risk factor was their childhood hGH treatment, Dr. Gargi Banerjee, lead study author and a clinical lecturer at University College London, said during the news conference.
The most common form of Alzheimer's is the sporadic version that affects 90% of patients and usually emerges after age 60 — there's no reason to think that this common form of the disease ever originates from clinical procedures, David Westaway, science programs director at the Institute for Neurodegenerative Diseases at the University of California, San Francisco, who was not involved in the research, told Live Science in an email.
Nonetheless, the study does suggest that, in very rare cases, Alzheimer's can spread in a similar way to a prion disease. In theory, accidental transmissions of Alzheimer's "seeds" could be possible in other medical procedures, so the study authors recommended that steps be taken to prevent that possibility, they wrote in the paper.
This article is for informational purposes only and is not meant to offer medical advice.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to community@livescience.com with the subject line "Health Desk Q," and you may see your question answered on the website!

Emily is a health news writer based in London, United Kingdom. She holds a bachelor's degree in biology from Durham University and a master's degree in clinical and therapeutic neuroscience from Oxford University. She has worked in science communication, medical writing and as a local news reporter while undertaking NCTJ journalism training with News Associates. In 2018, she was named one of MHP Communications' 30 journalists to watch under 30.
 Live Science Plus
Live Science Plus