Europeans' ancient ancestors passed down genes tied to multiple sclerosis, Alzheimer's risk
New research suggests that the risk of Europeans developing diseases such as multiple sclerosis and Alzheimer's stems from ancient human migrations.
Migrations of ancient humans in Eurasia may have impacted modern Europeans' risk of developing a variety of diseases, such as multiple sclerosis (MS), type 2 diabetes and Alzheimer's disease.
That's according to two new papers published Wednesday (Jan. 10) in the journal Nature. Along with two other articles from the same researchers, the papers include analyses of DNA from the bones and teeth of hundreds of ancient individuals, the oldest of whom date to the Mesolithic period, or Middle Stone Age. The scientists compared these people's DNA to the genomes of present-day Europeans.
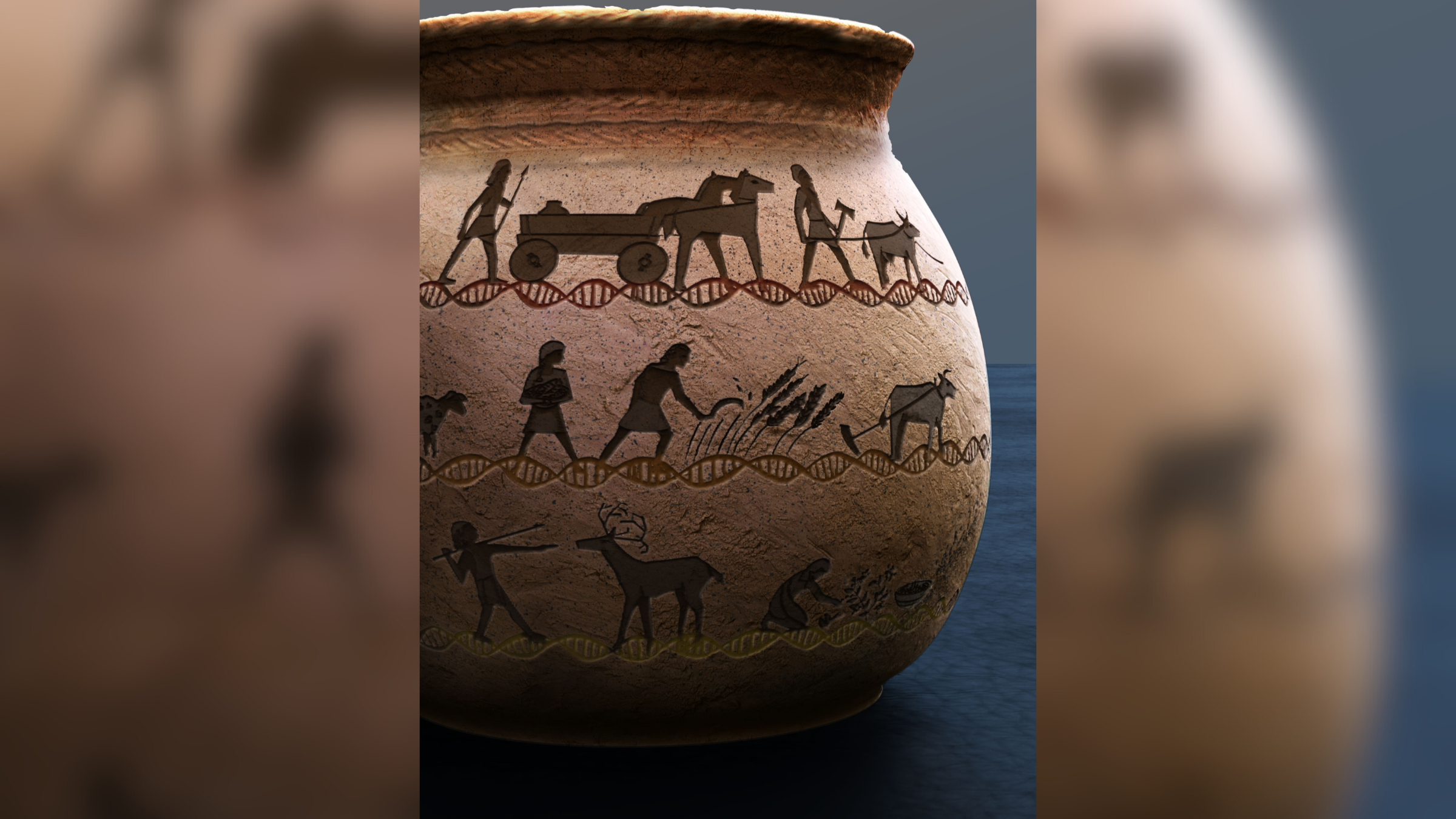
The project sheds light on the genetic legacy of three ancient human migrations into different regions of Europe: the arrival of hunter-gatherers around 45,000 years ago; Neolithic farmers from the Middle East approximately 11,000 years ago; and sheep and cattle farmers from the Pontic Steppe, a region that spans Eastern Europe and central Asia, around 5,000 years ago.
In all, the researchers compared the genomes of 1,750 ancient people with those of around 410,000 people who contributed data to a large repository called the U.K. Biobank. All the modern individuals self-identified as British and white, and the authors estimated how much ancient DNA was passed on to them.
Related: Largest-ever genetic family tree reconstructed for Neolithic people in France using ancient DNA
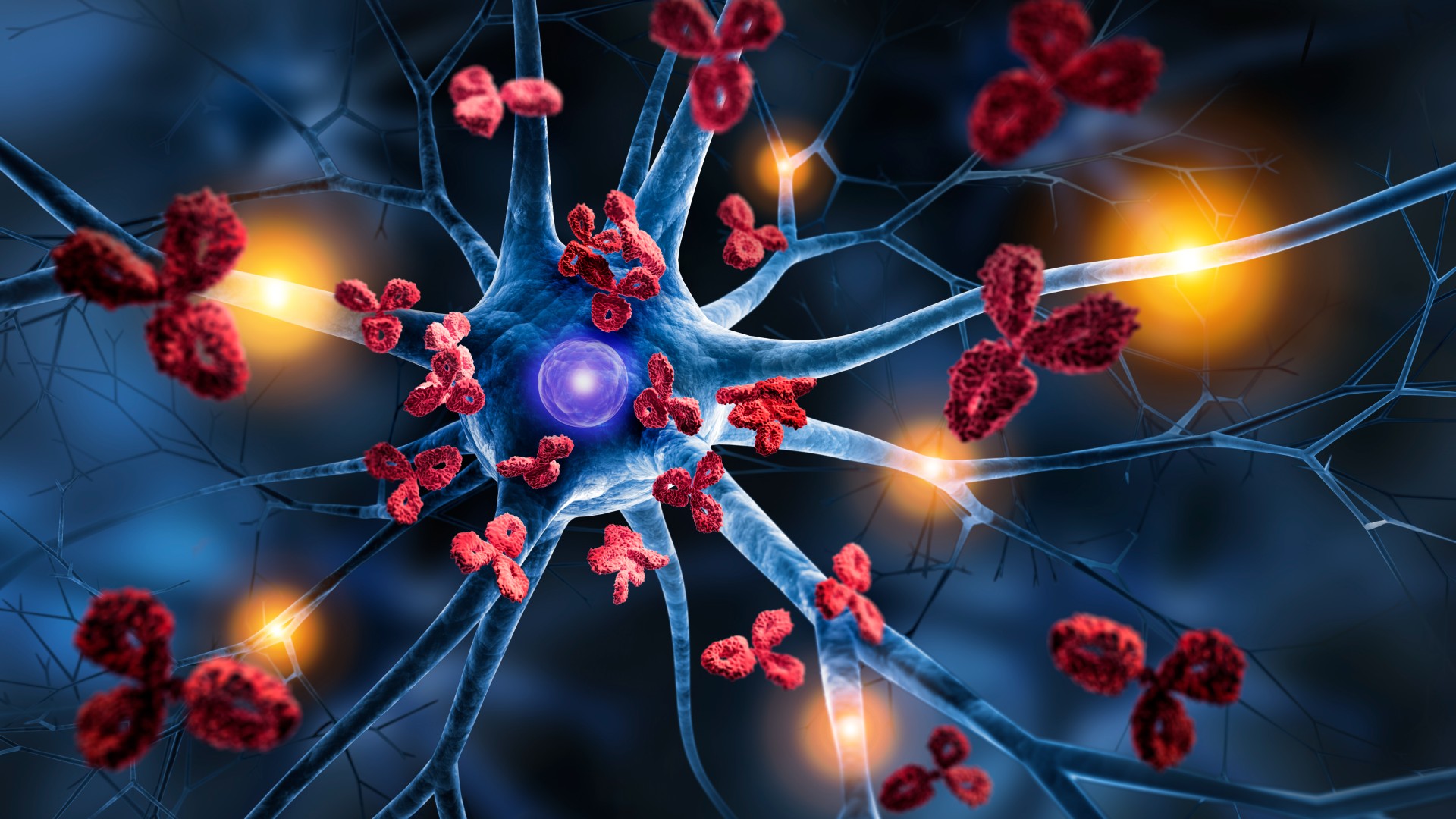
One of the new papers identified gene variants linked to the autoimmune disease MS that were carried by the Pontic Steppe farmers as they migrated mainly into northern Europe; this may help explain why the disease is most prevalent in people of Northern European descent. The researchers concluded these risk variants were "positively selected," meaning they offered some benefit to the migrants and were thus under evolutionary pressure to emerge.
Specific gene variants related to immune function are known to raise people's susceptibility to MS. These include HLA gene variants, which help the body spot pathogens. However, like a double-edged sword, certain HLA variants are also strongly associated with autoimmune diseases, where the body attacks its own cells.
Get the world’s most fascinating discoveries delivered straight to your inbox.
In the past, these variants potentially helped ancient farmers combat infectious diseases from their animals, the study authors theorize. However, as people's lifestyles changed over time, in terms of their hygiene, diets and medicine, the variants took on new meaning.
Understanding the evolutionary forces that drove these genes' selection could have implications for treating MS, the study authors hypothesize. Thinking about the double-edged sword, "what we need to move towards is to try to recalibrate the immune response," rather than completely eliminating it, Dr. Lars Fugger, co-senior study author and a professor of neuroimmunology at the University of Oxford in the U.K., said during a press conference on Jan. 9.
In another paper, the authors traced the inheritance of genetic risk variants for 35 complex traits, meaning those caused by a combination of many genes and their interactions with the environment. They discovered that genes associated with lactose tolerance in adults emerged in Europe around 6,000 years ago, and that Northern Europeans today may tend to be taller than Southern Europeans partly due to inheriting genes from the Pontic Steppe farmers.
They also found that people who carry more DNA from the hunter-gather group they studied may have a greater genetic risk of developing type 2 diabetes and Alzheimer's disease than people who carry fewer of those gene variants. Modern populations with this hunter-gather DNA largely live in Eastern Europe.
Related: 25,000-year-old human DNA discovered on Paleolithic pendant from Siberian cave
Alzheimer's risk variants may have been positively selected — for example, one risk variant called ApoE4 increases the risk of developing Alzheimer's but may boost fertility in women.
The fertility boost may have given our ancestors a "huge advantage," Dr. Astrid Iversen, co-senior study author and professor of virology and immunology at the University of Oxford, said during the conference.
"These articles add to the growing stack of evidence that dietary and lifestyle shifts, often accompanying migrations, may have favored alleles that have been maintained within the context of evolutionary trade-offs," Omer Gokcumen, a professor of evolutionary anthropology at the University at Buffalo in New York who was not involved in the research, told Live Science in an email.
These two studies looked for correlations between specific gene variants and the incidence of different diseases. Because of this, they can't prove that inheriting these ancient gene variants definitively causes these diseases in Europeans today.
"What these papers are doing is they're setting the framework of how you can use these ancient human genomes to understand the origins and spread of disease risk," Eske Willerslev, the director of the project and an evolutionary geneticist at the University of Cambridge and the University of Copenhagen, said during the press conference.
Editor's note: This article was updated on Jan. 15, 2024 with an updated quote from Omer Gokcumen. The story was first published on Jan. 10, 2024.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to community@livescience.com with the subject line "Health Desk Q," and you may see your question answered on the website!

Emily is a health news writer based in London, United Kingdom. She holds a bachelor's degree in biology from Durham University and a master's degree in clinical and therapeutic neuroscience from Oxford University. She has worked in science communication, medical writing and as a local news reporter while undertaking NCTJ journalism training with News Associates. In 2018, she was named one of MHP Communications' 30 journalists to watch under 30.
 Live Science Plus
Live Science Plus