Cystic Fibrosis: Causes, Symptoms and Treatment
Reference Article: Facts about cystic fibrosis.

Get the world’s most fascinating discoveries delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?

Delivered Daily
Daily Newsletter
Sign up for the latest discoveries, groundbreaking research and fascinating breakthroughs that impact you and the wider world direct to your inbox.

Once a week
Life's Little Mysteries
Feed your curiosity with an exclusive mystery every week, solved with science and delivered direct to your inbox before it's seen anywhere else.

Once a week
How It Works
Sign up to our free science & technology newsletter for your weekly fix of fascinating articles, quick quizzes, amazing images, and more

Delivered daily
Space.com Newsletter
Breaking space news, the latest updates on rocket launches, skywatching events and more!

Once a month
Watch This Space
Sign up to our monthly entertainment newsletter to keep up with all our coverage of the latest sci-fi and space movies, tv shows, games and books.

Once a week
Night Sky This Week
Discover this week's must-see night sky events, moon phases, and stunning astrophotos. Sign up for our skywatching newsletter and explore the universe with us!
Join the club
Get full access to premium articles, exclusive features and a growing list of member rewards.
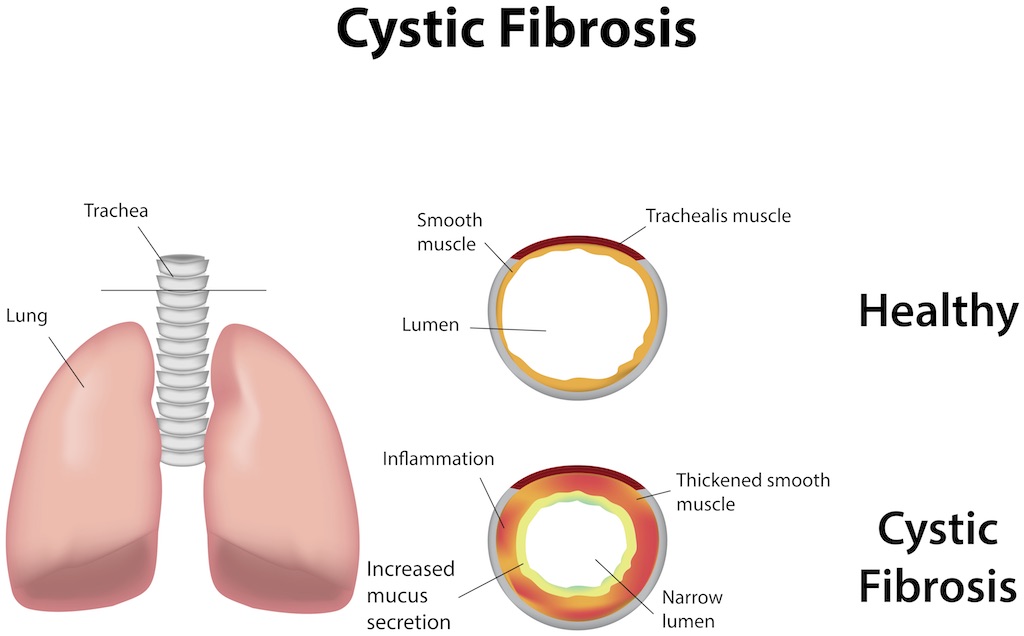
Cystic fibrosis is a genetic disorder that causes mucus-producing organs to malfunction and produce abnormally thick, sticky mucus. This causes problems in those organs, such as the lungs, the pancreas and the organs of the digestive system.
About 30,000 people in the United States have cystic fibrosis, and more than 75% of those affected are diagnosed by age 2, according to the Cystic Fibrosis Foundation.
In healthy people, mucus is thin and slippery. In people with cystic fibrosis, the substance is is abnormally thick and builds up in the lungs, making breathing difficult. Thick mucus also creates a breeding ground for bacteria, which can often lead to serious lung infections, said Dr. Mary Shannon Fracchia, a pediatric pulmonologist and co-director of the Cystic Fibrosis Center at MassGeneral Hospital for Children in Boston.
Too much thick mucus in the pancreas blocks the pathway for digestive enzymes to reach the intestines. Without these enzymes, the intestines can't properly absorb nutrients from food, leading to difficulty gaining weight and a slower growth rate in children with the disorder.
Besides affecting organs that produce mucus, cystic fibrosis also influences the sweat glands. People with the disease may have two to five times the normal amount of salt in their sweat, according to Children's Hospital of Pittsburgh. Parents may say they taste salt when kissing a child who has the disorder.
In some people, cystic fibrosis also harms the liver and reproductive system.
What causes cystic fibrosis?
The cause of cystic fibrosis is genetics, because a person needs to inherit a copy of a defective gene from both parents to develop the condition, Fracchia said. This defective gene, called the cystic fibrosis transmembrane conductance regulator (CFTR), was first identified in 1989, according to the Cystic Fibrosis Foundation.
Get the world’s most fascinating discoveries delivered straight to your inbox.
People with cystic fibrosis have a mutation in both copies of the CFTR gene (one copy inherited from each parent). People who have one copy of the defective CFTR gene, inherited from only one parent, become carriers of the disease. Carriers don't have any symptoms of cystic fibrosis, but they can pass the CFTR gene on to their children.
If both parents are carriers of cystic fibrosis and have a child, there is a 1 in 4 chance that the child will have the disease, Fracchia told Live Science.
The defective CFTR gene produces a faulty protein that affects the movement of chloride — a component of salt, or sodium chloride — across cell membranes, according to the Cystic Fibrosis Foundation. This alters the flow of salt and water into and out of cells, causing problems in glands that produce mucus and sweat.
The CFTR gene is most common in white people of Northern European descent, but other ethnic populations can also develop the disease.
What are cystic fibrosis symptoms?
The lungs and pancreas are the organs most affected by cystic fibrosis, leading to breathing and digestive problems. Symptoms of cystic fibrosis can vary from one person to another, depending on the severity of the disease.
According to the Cystic Fibrosis Foundation, symptoms and complications may include:
Respiratory symptoms
- Frequent lung infections, such as pneumonia or bronchitis.
- Persistent coughing that produces thick, heavy mucus.
- Wheezing or shortness of breath.
- Nasal congestion and nasal polyps (small growths in the nose).
- Frequent sinus infections (sinusitis).
Digestive symptoms
- Poor absorption of dietary protein, which may slow growth and weight gain in children.
- Poor absorption of dietary fats, which can make stools appear greasy and bulky.
- Deficiencies of fat-soluble vitamins (vitamins A, D, E and K) due to low levels of pancreatic enzymes.
- Chronic constipation.
- Stomach pain.
- Pancreatitis, or inflammation of the pancreas.
- Diabetes from damage to pancreatic cells that produce insulin.
Sweat gland complications
- Salty-tasting skin when kissed.
- Excessive sweating on hot days.
Reproductive complications
- Males may have blockages of the sperm canal because of thick mucus clogging the vas deferens (the tube that carries sperm to the penis), leading to infertility.
- Women may have thick cervical mucus, making it harder to become pregnant.
How is cystic fibrosis diagnosed?
A blood test for cystic fibrosis is first performed at birth. A blood sample is checked for certain biomarkers of the disease as part of routine newborn screening in all 50 states, according to the Mayo Clinic. If there is a positive result, doctors will perform a genetic test to confirm diagnosis.
Once the infant is at least 2 weeks old, doctors may follow up with a sweat test, which measures the amount of chloride in sweat collected from a small area of skin. People with the disease have higher than normal amounts of chloride in their sweat.
Other diagnostic tests may be done depending on a person's symptoms; these tests can include pancreatic function tests, chest X-rays and pulmonary function tests to measure how well the lungs work.
Treatment for cystic fibrosis
The main goals of treatment for cystic fibrosis are to prevent and treat infections, keep lungs and airways as clear as possible, and maintain adequate calories and nutrition, according to Children's Hospital of Pittsburgh.
Every year, the life expectancy for people with cystic fibrosis is getting longer, Fracchia told Live Science. The current life expectancy for someone with the disease is 41 to 42 years, Fracchia said.
According to the Mayo Clinic, treatment for lung problems may include:
- Daily chest physical therapy to help loosen and clear thick mucus in the lungs and airways. This can be done by a physical therapist or a parent and involves gently pounding on the back or chest to break up mucus, Fracchia said. Sometimes, this therapy is done by wearing a vest that vibrates to loosen mucus, she said.
- Taking medication to decrease inflammation and swelling in the lungs and to thin mucus.
- Using inhaled medications (bronchodilators) can open airways and improve breathing.
- Getting regular exercise to loosen mucus in the airways, stimulate coughing and improve physical conditioning.
- Taking antibiotics to treat and prevent lung infections.
Treatment for digestive problems may include:
- Eating a high-calorie, high-fat diet and taking vitamin supplements.
- Taking pancreatic enzymes with every meal and snack to help digest food and absorb nutrients.
Additional resources:
- Learn more about the genetics of cystic fibrosis and carrier testing, from the University of California, San Francisco.
- Find out how cystic fibrosis affects kids, from kidshealth.org.
- Learn what's it like to be a young adult with cystic fibrosis in this article by Gunnar Esiason for CNN Health.
This article is for informational purposes only, and is not meant to offer medical advice.
Cari Nierenberg has been writing about health and wellness topics for online news outlets and print publications for more than two decades. Her work has been published by Live Science, The Washington Post, WebMD, Scientific American, among others. She has a Bachelor of Science degree in nutrition from Cornell University and a Master of Science degree in Nutrition and Communication from Boston University.
 Live Science Plus
Live Science Plus