What is Bariatric Surgery?
Bariatric surgery is a surgical operation on the stomach and intestine used to treat obesity. It is an option for people who are still severely obese after attempting to lose weight through other methods, such as diet and exercise, or who have a serious health condition related to their obesity, such as type 2 diabetes.
Weight-loss surgery: How it works
Bariatric surgery makes the stomach smaller — either by restricting the size of the stomach with a band, or physically removing a portion of the stomach with surgery. A smaller stomach means patients eat less, which leads to weight loss. Some types of bariatric surgery also reduce the absorption of food by the body, which also contributes to weight loss. And studies show that some producers cause a change in the level of the hormone that regulates appetite, making people feel less hungry.
Many patients who have weight loss surgery participate in a program that provides support before, during and after surgery, which can help patients maintain weight loss, said Dr. Miguel Burch, associate director of Minimally Invasive Surgery at Cedars-Sinai in Los Angeles. Among patients with good support programs, 85 to 90 percent achieve more than 50 percent weight loss, and keep it off for more than five years, Burch said. However, without a good support program in place, the chances of gaining weight back would be higher, he said.
The best outcomes occur in people who eat a healthy diet and engage in regular exercise after surgery, according to the National Institute of Diabetes and Digestive Kidney Diseases (NIDDK). Patients should also maintain high levels of protein in their diet, so that they will lose more fat mass and less muscle mass, Burch said.
Who's eligible for surgery?
People are eligible for bariatric surgery if they have a body mass index (BMI) of 40 or more, or if they have a serious health problem related to their obesity and have a BMI of 35 or more, according to the NIDDK. People with a BMI of 30 or more are eligible for an adjustable gastric band (one type of bariatric surgery) if they also have at least one health problem linked with obesity.
Anyone thinking about having this surgery should understand the possible risks and benefits of the procedure, and how their life may change afterwards, the NIDDK says.
People who are not prepared to make lifestyle changes, which often include a change in diet, are not good candidates for the surgery, Burch said.
Get the world’s most fascinating discoveries delivered straight to your inbox.
"Patients who really just look at the surgery as something magical that will help them lose the weight," are probably not ready for surgery, Burch said.
Types of surgery
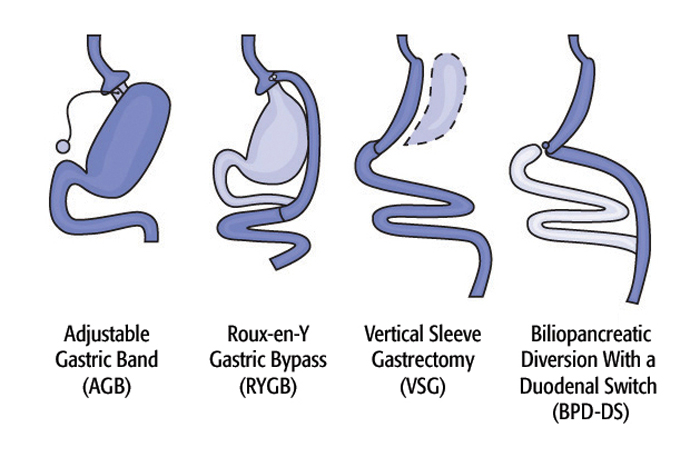
There are four main types of bariatric surgery offered in the United States: adjustable gastric band, Roux-en-Y gastric bypass, biliopancreatic diversion with a duodenal switch, and vertical sleeve gastrectomy.
An adjustable gastric band (AGB) is a band that's placed around the top of the stomach, which reduces hunger and limits food intake. Some advantages of the band are that it is a reversible procedure, usually requires a short hospital stay, and has the lowest risk of vitamin deficiencies, according to the American Society for Metabolic and Bariatric Surgery. Some disadvantages of the band are that weight loss can be slower than with other types of surgery, and that a small percentage of patients may have complications such as having the band slip out of place or erode into the stomach, the ASMBS says.
Roux-en-Y gastric bypass (RYGB) is a surgery that creates a small pouch out of the top of the stomach, and connects it to part of the small intestine called the jejunum. In this way, food bypasses part of the stomach and the duodenum — the first part of the small intestine. Some advantages of gastric bypass are that it can produce significant weight loss (60 to 80 percent of excess weight), and that it may produce changes in gut hormones that reduce appetite, ASMBS says. However, it usually requires a longer hospital stay than that of the AGB procedure.
Biliopancreatic diversion with a duodenal switch (BPD-DS) removes a large portion of the stomach, but leaves a short part of the duodenum, which is then connected to the lower part of the small intestine. This procedure limits the amount of food, vitamins and minerals that are absorbed, which can help with weight loss, but can also increase the risk for long-term problems such as anemia or osteoporosis, the NIDDK says.
A vertical sleeve gastrostomy (VSG) removes most of the stomach (80 to 85 percent), and this smaller stomach limits the amount of food eaten. Advantages of the sleeve gastrostomy include that it produces rapid weight loss (more than 50 percent), and does not require a re-routing of the food system, according to ASMBS. But like gastric bypass and biliopancreatic diversion, it is a non-reversible procedure.
Most surgeries done today are laparoscopic, meaning that doctors make small cuts in the belly to insert surgical tools, and use a camera to guide the surgery (as opposed to making one large cut to open up the belly, which is referred to as "open" surgery.)
Surgery risks
According to the NIDDK, risks of the surgical procedure include: infection, bleeding, leaks from the places where the intestines are sewn together, and blood clots that can move to the lungs and heart.
At high-quality surgery centers, leaks happen in less than 1 percent of patients, Burch said.
A more common side effect is mild dehydration because the stomach holds less liquid than it did before, Burch said, but most patients can quickly make accommodations to reduce this risk.
Poor absorption of nutrients is also a risk, and patients often need to take vitamins and minerals. If not addressed, lack of certain vitamins can lead to diseases, including pellagra (caused by lack of Vitamin B3/niacin) and beri beri (caused by lack of vitamin B1/thiamine.) Nowadays, most people who undergo weight loss surgery do not experience malnutrition or low vitamin levels, because patients take vitamins after weight loss surgery, Burch said.
Recent studies also suggest that weight loss surgery can increase the risk of alcohol abuse in a small percentage of patients. In a 2012 study published in the Journal of the American Medical Association involving 2,000 people who'd had weight loss surgery, the percentage of those reporting symptoms of alcohol abuse increased from 7.6 percent before surgery to 9.6 percent two years after surgery. Although the reason for this risk is not known, some researchers say the surgery increases a person's sensitivity to alcohol.
Benefits of surgery
In addition to weight loss, bariatric surgery may help improve certain conditions tied to obesity, such as heart disease, high blood pressure and sleep apnea, according to the Mayo Clinic.
Studies also suggest that gastric bypass surgery can reverse type 2 diabetes. A 2011 study in the journal Science Translational Medicine said that about 50 to 80 percent of patients who have gastric bypass surgery experience a reduction in their blood sugar levels that's enough for them to be considered free of type 2 diabetes. This can happen very soon after surgery.
Weight loss surgery may also help with infertility. In a small 2011 study, 6 infertile women with polycystic ovarian syndrome (PCOS), a condition that can cause infertility and often presents with weight gain, became pregnant within three years of weight loss surgery. However, weight loss surgery is not typically recommended as a treatment for infertility, Dr. Beth Plante, a clinical assistant professor of obstetrics and gynecology at Brown University Medical School, told Live Science in a 2011 interview. Rather, weight loss surgery may be one way that PCOS patients chose to lose weight, Plante said.
Perhaps the biggest benefit of weight loss surgery is improvement in quality of life, Burch said. Some people are able to perform activities that they could not before surgery, such as running around with their children, Burch said.
Follow Rachael Rettner @RachaelRettner. Follow Live Science @livescience, Facebook & Google+

Rachael is a Live Science contributor, and was a former channel editor and senior writer for Live Science between 2010 and 2022. She has a master's degree in journalism from New York University's Science, Health and Environmental Reporting Program. She also holds a B.S. in molecular biology and an M.S. in biology from the University of California, San Diego. Her work has appeared in Scienceline, The Washington Post and Scientific American.
 Live Science Plus
Live Science Plus





