'Superbugs' can linger in the body for years, potentially spreading antibiotic resistance
People can carry some antibiotic-resistant strains of bacteria for up to nine years, new research suggests.
Get the world’s most fascinating discoveries delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?

Delivered Daily
Daily Newsletter
Sign up for the latest discoveries, groundbreaking research and fascinating breakthroughs that impact you and the wider world direct to your inbox.

Once a week
Life's Little Mysteries
Feed your curiosity with an exclusive mystery every week, solved with science and delivered direct to your inbox before it's seen anywhere else.

Once a week
How It Works
Sign up to our free science & technology newsletter for your weekly fix of fascinating articles, quick quizzes, amazing images, and more

Delivered daily
Space.com Newsletter
Breaking space news, the latest updates on rocket launches, skywatching events and more!

Once a month
Watch This Space
Sign up to our monthly entertainment newsletter to keep up with all our coverage of the latest sci-fi and space movies, tv shows, games and books.

Once a week
Night Sky This Week
Discover this week's must-see night sky events, moon phases, and stunning astrophotos. Sign up for our skywatching newsletter and explore the universe with us!
Join the club
Get full access to premium articles, exclusive features and a growing list of member rewards.
Antibiotic-resistant bacteria that pose a critical threat to public health can remain in the body for nearly a decade.
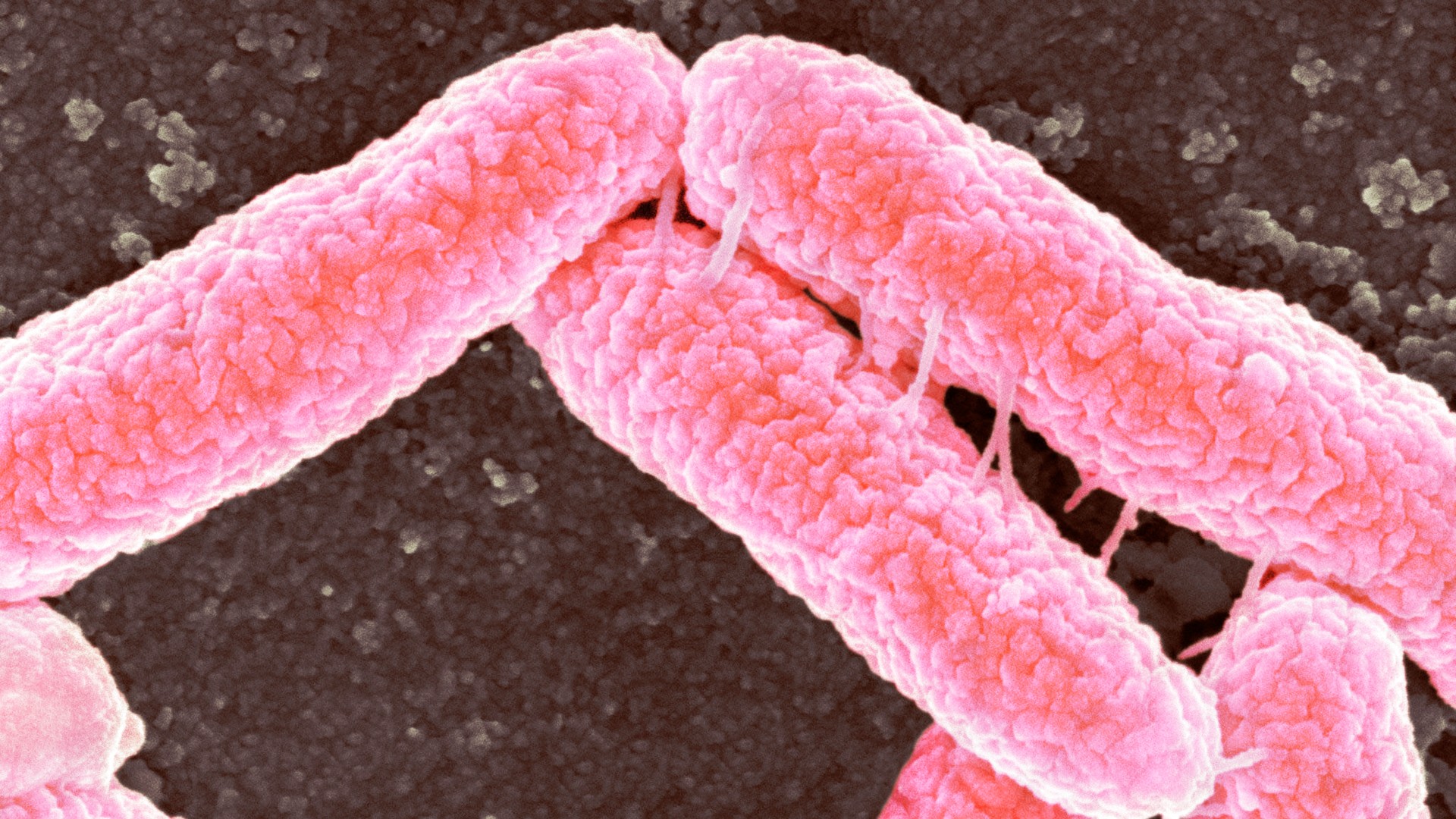
That's according to a new analysis of two antibiotic-resistant strains of the bacteria Klebsiella pneumoniae and Escherichia coli sampled from more than 70 hospital patients in Basel, Switzerland. The patients were screened for the presence of the bacteria in their body over the course of 10 years.
K. pneumoniae and E. coli can cause a range of serious infections, such as pneumonia, blood poisoning and urinary tract infections. The overuse of antibiotics pushes bacteria to evolve resistance to the drugs, with serious health implications. The two bacterial species featured in the new study belong to a broad group called Enterobacterales, which are particularly affected by beta-lactam antibiotics such as penicillins and cephalosporins.
Drug-resistant bacteria can colonize the body, meaning that they are found within it but don't cause harm, or they can trigger full-blown infection under certain circumstances. Until now, little was known about how long these resistant bacteria stay in people's bodies and whether their genetic makeup changes over time.
Related: Dangerous 'superbugs' are a growing threat, and antibiotics can't stop their rise. What can?
Now, in a study published Dec. 21 in the journal Nature Communications, scientists have revealed that the same strains of resistant K. pneumoniae and E. coli can stay in a patient's body for up to five or nine years, respectively. As these colonizing bacteria can trigger disease, carriers could be at a prolonged risk of experiencing recurrent infections and of potentially exposing others to the microbes, the authors say.
"These patients not only repeatedly become ill themselves, they also act as a source of infection for other people — a reservoir for these pathogens," Lisandra Aguilar-Bultet, lead study author and a research associate in microbial genomics and bioinformatics at the University Hospital of Basel in Switzerland, said in a statement. For instance, resistant bacteria can be spread via poor hygiene practices, close person-to-person contact or exposure to contaminated medical instruments.
Get the world’s most fascinating discoveries delivered straight to your inbox.
For the study, the researchers genetically screened 76 samples of resistant K. pneumoniae and 284 samples of E. coli that were collected from patients who were known to carry the bacteria. The patients were screened each time they were admitted to the University Hospital Basel between 2008 and 2018.
Most samples were taken as part of routine screening upon hospital admission for any condition, but 12.5% of them were collected because the person had a suspected infection with these specific bacteria. During the study period, an average of four samples of both resistant K. pneumoniae and E. coli were taken from each patient, mainly via rectal swabs.
Over the years, the genetic diversity of the bacteria in the patients bodies remained low: the same strains of resistant K. pneumoniae stayed in the bodies of all patients who were originally infected with the bacteria, while 84% of patients remained colonized with the same strains of resistant E. coli.
Overall, the longest time that any strain of resistant bacteria stayed in a person's body was 1,704 days for K. pneumoniae and 3,387 days for E. coli. The researchers also often found the same strain of either colonizing or infectious bacteria in different parts of a given patient's body.
Furthermore, the same antibiotic resistance genes were often shared by different strains of bacteria within the same person. This suggests that the bacteria are passing these genes to each other, the authors said, which could contribute to the transmission of antibiotic resistance. Such gene swapping, known as horizontal gene transfer, is a well-known mechanism by which microbes gain antibiotic resistance.
The study's findings set the groundwork for future research to uncover why these resistant bacteria stay in the body so long and what makes them switch from simply colonizing the body to causing full-blown infections, the authors said.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to community@livescience.com with the subject line "Health Desk Q," and you may see your question answered on the website!

Emily is a health news writer based in London, United Kingdom. She holds a bachelor's degree in biology from Durham University and a master's degree in clinical and therapeutic neuroscience from Oxford University. She has worked in science communication, medical writing and as a local news reporter while undertaking NCTJ journalism training with News Associates. In 2018, she was named one of MHP Communications' 30 journalists to watch under 30.
 Live Science Plus
Live Science Plus