How to Fight Viral Epidemics in the Future
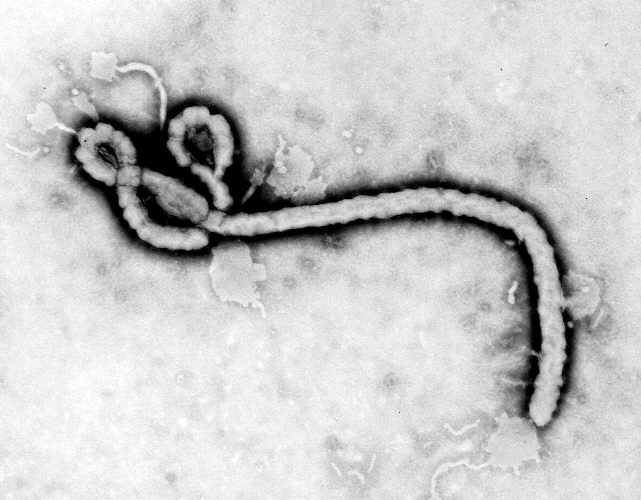
Emerging viral diseases are at the center of health news right now. The most significant of them, in terms of human cases and death toll, is the re-emergence of Ebola virus, which is causing the biggest outbreak of the disease in history. But there is also chikungunya fever, which appeared in the United States for the first time in July, and enterovirus D68, a previously rare disease causing an outbreak of respiratory illness among U.S. children.
Humans have come a long way in preventing viral diseases over the last century. Today, children in the U.S. routinely receive vaccinations against nine viral diseases, including many that used to cause life-threatening complications, such as polio.
But still, there are fewer treatments for viral diseases than for those caused by bacteria, and when infectious disease pandemics emerge, the pathogens that are the most lethal are the viruses, experts say.
How will humans protect themselves against viruses in the future? Experts are working on ways to find new drug treatments, as well as to prevent epidemics from emerging in the first place. [5 Most Likely Real-Life Contagions]
Viral treatments lag behind
Treatments for viral diseases have generally lagged behind treatments for bacterial diseases, experts say. One reason for that is simply because scientists have been working on antibacterial treatments for longer, said Paul Roepe, co-director of Georgetown University's Center for Infectious Disease.
"We knew about a lot more bacterial diseases before we knew about viral disease," Roepe said.
Get the world’s most fascinating discoveries delivered straight to your inbox.
Viruses are also much smaller than bacteria — about 100th the size — and they have fewer genes or proteins to target with treatments.
"Viruses are inherently difficult targets," for modern medicine, said Derek Gatherer, a bioinformatics researcher at Lancaster University in the United Kingdom. "They have, in general, smaller genomes than bacteria," so there are fewer places to look for ways to combat them, he said.
Viruses also mutate much more quickly than bacteria, so any therapy that is developed may no longer work after a short time, Gatherer said.
In addition, bacteria are living cells that divide on their own, and a lot of drug treatments against bacteria work by knocking out essential functions of those cells, such as the ability to replicate, Roepe said.
But viruses are not made of cells, and they are even not exactly alive — they hijack the machinery of their hosts' cells in order to replicate, so researchers can't target virus functions or replication in a traditional way.
"When you're trying to close in or 'kill' a virus, you're really trying to kill host cell machinery," Roepe said.
'Antibiotics' for viruses?
When the first antibiotics were developed in the 1940s, they were considered a miracle cure for diseases. A few decades later, scientists developed drugs against viruses, known as antivirals.
However, although there are "broad-spectrum" antibiotics, which are single drugs that work against dozens of bacteria, the spectrum for antivirals is much narrower, Roepe said. Most antiviral drugs are specific for one type of virus, although some work against two or three.
Some of the most successful antiviral drugs inhibit a certain viral enzyme called reverse transcriptase, which synthesizes parts of the virus, Roepe said. Several drugs against HIV work in this way.
However, only RNA viruses (such as HIV and Ebola) use reverse transcriptase, so drugs against this enzyme will not work for DNA viruses, Roepe said. In addition, the structure of reverse transcriptase can be very different depending on the virus, which is why an antiviral that works against HIV might not work for Ebola.
Discovering new drugs
The good news is that discovering antiviral drugs is easier today than it used to be, thanks to new technologies.
A few decades ago, researchers had to test potential drugs individually, and it could take three to six months to test 100 potential drugs, Roepe said. But today, the process is automated with robots, so those same 100 drugs would require only a few days to test, he said.
In addition, researchers can now view three-dimensional models of viral components on a computer, and quickly design and "test" compounds with computer programs that simulate the binding of drugs to viral components.
Such "in silico" drug design has improved in recent years, and will play an important role in future drug discoveries, Roepe said.
Preventing pandemics
But because new antiviral drug treatments may be years or decades away, public health organizations are focused on stopping pandemics before they start.
"The future of dealing with viral pandemics is, we're going to be able to prevent them," said Dr. Peter Daszak, a disease ecologist and the president of EcoHealth Alliance, a nonprofit organization that works to prevent emerging diseases.
New viral diseases typically emerge because of human activity that brings people into contact with wildlife, such as road building, hunting and agriculture expansion, Daszak said. About 75 percent of emerging diseases in people come from animals, according to EcoHealth Alliance.
So to reduce the risk of an outbreak, researchers need to figure out ways to reduce the activity that brings us into contact with wildlife, particularly in "hotspots" where diseases tend to emerge, such as tropical areas, Daszak said.
"In West Africa, where Ebola emerged, there's one original case," Daszak said. "If you can identify the activity that allows the first case to happen, and reduce that activity, you reduce the risk of an outbreak."
Although it's not clear how the current Ebola outbreak started, some people have speculated that handling bats — a suspected reservoir of Ebola — may have played a role.
Daszak and colleagues are working on several projects to prevent outbreaks, including a project in Malaysia to move tree logging to lower-risk areas, (such as areas that have already been logged and re-planted) so people don't move into new regions of tropical forest.
"The approaches are not as high tech [as drug discovery], but they're really necessary," to prevent pandemics, Daszak said.
Follow Rachael Rettner @RachaelRettner. Follow Live Science @livescience, Facebook & Google+. Original article on Live Science.

Rachael is a Live Science contributor, and was a former channel editor and senior writer for Live Science between 2010 and 2022. She has a master's degree in journalism from New York University's Science, Health and Environmental Reporting Program. She also holds a B.S. in molecular biology and an M.S. in biology from the University of California, San Diego. Her work has appeared in Scienceline, The Washington Post and Scientific American.


