HPV vaccination drives cervical cancer rates down in both vaccinated and unvaccinated people
Researchers have found that human papillomavirus (HPV) vaccines are highly effective at reducing cervical cancer-causing infections and can offer herd immunity, reinforcing previous research and highlighting the need for a global HPV vaccine rollout.

Get the world’s most fascinating discoveries delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?

Delivered Daily
Daily Newsletter
Sign up for the latest discoveries, groundbreaking research and fascinating breakthroughs that impact you and the wider world direct to your inbox.

Once a week
Life's Little Mysteries
Feed your curiosity with an exclusive mystery every week, solved with science and delivered direct to your inbox before it's seen anywhere else.

Once a week
How It Works
Sign up to our free science & technology newsletter for your weekly fix of fascinating articles, quick quizzes, amazing images, and more

Delivered daily
Space.com Newsletter
Breaking space news, the latest updates on rocket launches, skywatching events and more!

Once a month
Watch This Space
Sign up to our monthly entertainment newsletter to keep up with all our coverage of the latest sci-fi and space movies, tv shows, games and books.

Once a week
Night Sky This Week
Discover this week's must-see night sky events, moon phases, and stunning astrophotos. Sign up for our skywatching newsletter and explore the universe with us!
Join the club
Get full access to premium articles, exclusive features and a growing list of member rewards.
Human papillomavirus (HPV) vaccines can dramatically reduce the rate of infections that cause cervical cancer, even in people who haven't been vaccinated, a new long-term study reveals.
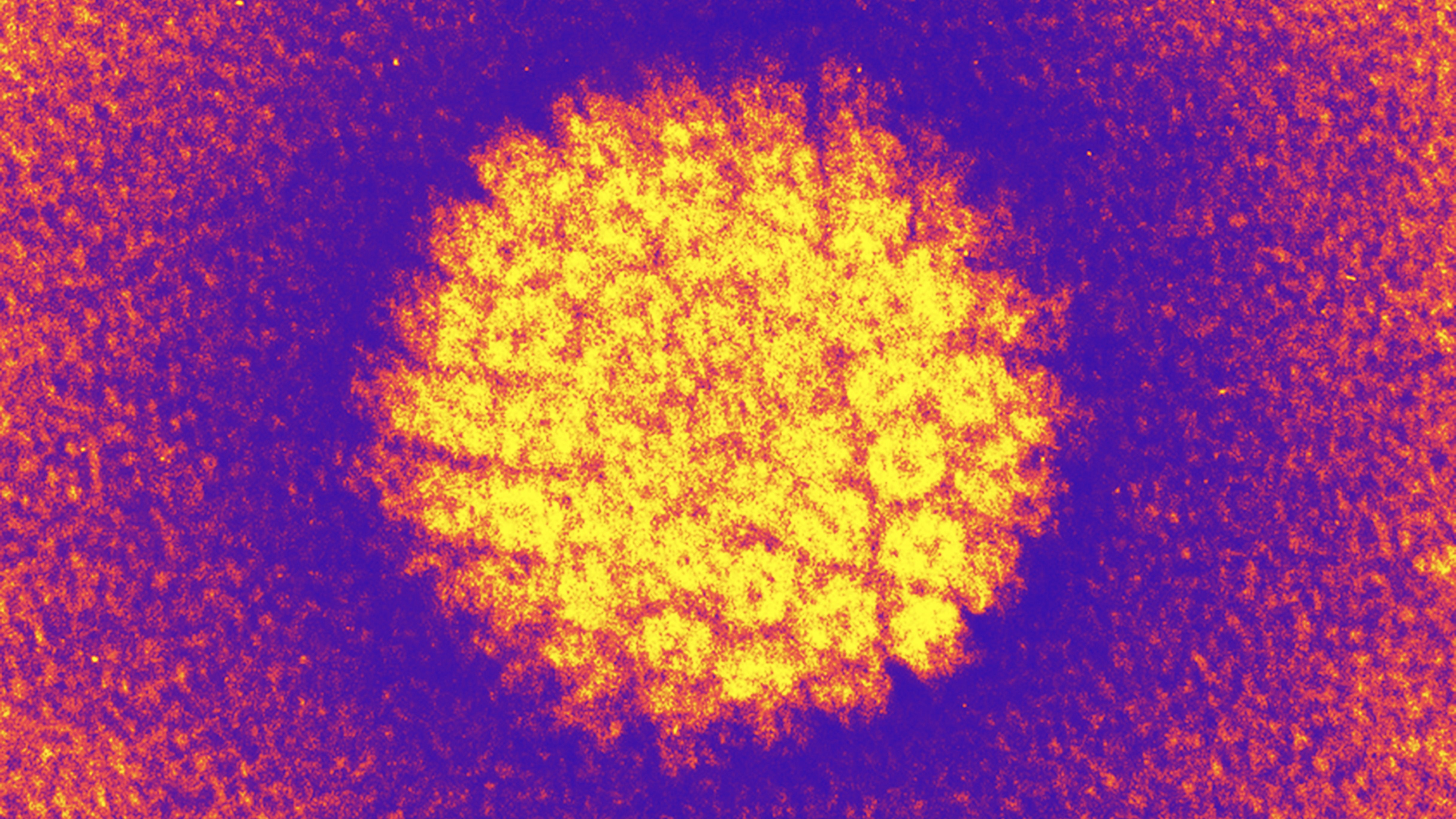
Most cases of cervical cancer are caused by high-risk HPV viruses, which can drive changes in cells that turn them cancerous. Two types of high-risk HPV are most likely to cause cervical cancer. After the introduction of HPV vaccines in the U.S., the shots reduced the amount of people testing positive for those cervical-cancer-causing viruses by a whopping 98.4% in vaccinated teens and young women in Cincinnati, the focus of the new study. Meanwhile, in unvaccinated people of the same age, the rates of infection still fell by 71.6% in the same time period.
This demonstrates that HPV vaccines, introduced in the U.S. in 2006, can lead to herd immunity, which is when a population becomes so resistant to the spread of a virus that even unvaccinated people are indirectly protected.
HPV is the most common sexually transmitted infection worldwide; that stat includes both low- and high-risk strains. While it's primarily known for its potential to cause cervical cancer, exposure to high-risk HPV can also lead to other cancers in both sexes, according to a statement released by the researchers. These include those affecting the anus, head and neck.
Scientists have known for many years that HPV vaccines are highly effective, significantly reducing the rate of cervical precancers in young U.S. women and preventing cervical cancer deaths. However, the new 17-year study, published Monday (Sept. 29) in the journal JAMA Pediatrics, found that the vaccines have also reduced high-risk cervical infections in adolescent girls and young women at increased risk of HPV, even when they themselves were not vaccinated.
Nearly all sexually active people get HPV at some point in their lives. The infections are typically symptomless and tend to go away on their own within two years. However, in some cases, they can persist and ultimately cause cancers.
A 2020 study published in The Lancet Global Health estimated that in 2018, there were 690,000 cases of cancer attributed to HPV worldwide, including 620,000 in women and 70,000 in men. Cervical cancer accounted for about 80% of these cancer cases. So while most people don't get cancer as a result of an HPV infection, the virus' prevalence makes it a major public health problem.
Get the world’s most fascinating discoveries delivered straight to your inbox.
In the new study, the researchers analyzed data from six surveillance studies in Cincinnati, collected from 2006 — the year before the vaccine became available there — to 2023. The study included 2,335 adolescent girls and young women between 13 and 26 years old. They focused primarily on participants who had an increased risk for HPV because they had multiple sexual partners or a history of sexually transmitted infection.
Multiple HPV vaccines have been introduced since 2006, and this study assessed the effectiveness of three versions: the 2-valent version, which guards against HPV 16 and HPV 18, the HPV responsible for more than 70% of cervical cancers; the 4-valent version, which additionally covers HPV 6 and HPV 11; and the 9-valent versions, which protect against another five types.
During the study period, the rate of HPV infections fell as the vaccines became available and the proportion of vaccinated participants increased, from 0% to 82%. Infections covered by the 2-valent vaccine dropped by 98.4% among vaccinated individuals, while the remaining HPV types covered by the 4-valent and 9-valent vaccines dropped by 94.2% and 75.7%, respectively.
The 9-valent vaccine was just as protective as the 2-valent and 4-valent vaccines in clinical trials, lead study author Dr. Jessica Kahn, a professor of pediatrics at the Albert Einstein College of Medicine in New York, told Live Science. But the decline in virus types targeted by the 9-valent vaccine was lower in this real-world scenario because it was licensed more recently, meaning fewer participants had received at least one dose of that version by the time of the study.
Among unvaccinated participants, HPV 16 and HPV 18 infections dropped by 71.6% in the study population, while the remaining two strains covered by the 4-valent vaccine dropped by 75.8%, indicating a high degree of herd immunity. The researchers didn't have enough data to effectively look at all the strains covered by the newer 9-valent vaccine in unvaccinated people.
The findings are good news for highly vaccinated areas, but rates of cervical cancer are higher in poorer countries than in the U.S. Globally, only 31% of adolescent girls and 8% of adolescent boys between 9 and 14 years old have received one dose of an HPV vaccine, according to 2024 World Health Organization data, the latest available. Increasing vaccine uptake worldwide could have dramatic impacts.
"By expanding uptake of this highly safe and effective vaccine, and ensuring access to screening and treatment, we can achieve one of the greatest public health victories of our time: the elimination of cervical cancer worldwide," Kahn said.
This article is for informational purposes only and is not meant to offer medical advice.

Patrick Pester is the trending news writer at Live Science. His work has appeared on other science websites, such as BBC Science Focus and Scientific American. Patrick retrained as a journalist after spending his early career working in zoos and wildlife conservation. He was awarded the Master's Excellence Scholarship to study at Cardiff University where he completed a master's degree in international journalism. He also has a second master's degree in biodiversity, evolution and conservation in action from Middlesex University London. When he isn't writing news, Patrick investigates the sale of human remains.
You must confirm your public display name before commenting
Please logout and then login again, you will then be prompted to enter your display name.
 Live Science Plus
Live Science Plus










