Varicose Veins & Spider Veins: Causes & Treatment

Varicose veins are spidery, swollen veins that bump out from beneath the skin. They are usually red or blue and typically appear on the legs, but can also be found in other parts of the body. Smaller varicose veins are called spider veins.
Having varicose veins is common, and women develop them more often than men. They are usually harmless, but in some people, they can lead to serious problems, such as leg swelling and pain, blood clots and skin changes, according to the National Institutes of Health.
Causes
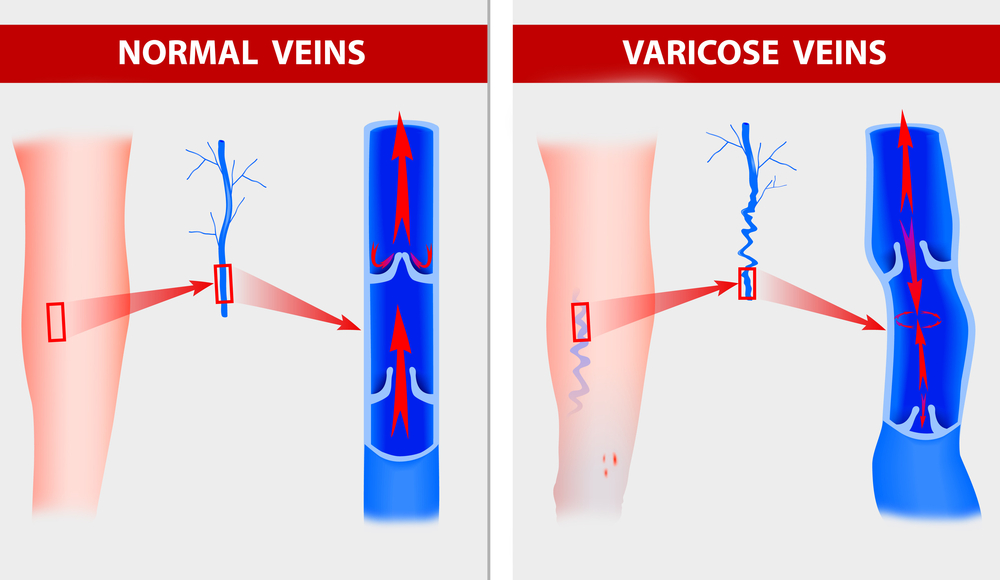
In healthy veins, blood normally flows from the periphery of the body to the central venous system and up to heart, from where it gets pumped to the lungs to be reoxygenated, said Dr. Lowell Kabnick, a vascular expert and director of the Vein Center at NYU Langone Medical Center, in New York.
Veins have valves that keep the blood moving in one direction. "When a vein is diseased or gets enlarged, the valve cuffs don’t work any more," Kabnick told Live Science. Blood starts to back up, and the result is a varicose vein — "a dilated or enlarged vein that looks ropey, with blood that is flowing in the opposite direction as blood should flow," he said.
The venous systems has superficial veins, which are close to the skin and have many branches, and deep veins, which are closer to the bones and connect to veins leading to the heart. Varicose veins most often form along superficial veins, where they are usually not harmful to a person's health, Kabnick said. But in rare cases, varicose veins can develop into more serious problems that require intervention, he added. [Related: Circulatory System: Facts, Function & Diseases]
The NIH lists these factors that affect the risk of developing varicose veins:
- older age
- being female
- congenital valve defects
- obesity
- pregnancy
- history of blood clots in the legs
- standing or sitting for long periods
- family history of varicose veins
Hormonal changes such as puberty, pregnancy and menopause, as well as birth control or hormone replacement, can also increase the risk.
Get the world’s most fascinating discoveries delivered straight to your inbox.
Symptoms
Symptoms of varicose veins include feelings of fullness, heaviness or aching in the legs, visibly swollen veins, mild swelling of the ankles or feet, pain, itching, or fatigue, Kabnick said. Complications of the condition can include discoloration of skin, inflammation under the skin, thinning of the skin or breakdown/ulceration of the skin, he said. In rare cases, blood clots can form. If they form in deep veins, they can break off and travel to the lungs, which is much more dangerous, Kabnick said.
Tests
Those who suspect they may have varicose veins should consult a doctor, who can look for swelling, changes in skin color or sores on the legs. A doctor may also check venous blood flow and check for other problems, such as blood clots.
For example, a doctor may use duplex ultrasound, an imaging method that reveals which way blood is flowing in a vein. If it's flowing against the direction it should be, the vein is probably varicose, Kabnick said.
Treatment
According to the NIH, doctors may recommend the following self-care measures for managing varicose veins:
- wearing compression stockings to reduce swelling
- avoiding sitting or standing for long periods
- raising your legs above your heart for 15 minutes three to four times per day
- treating any open sores or infections
- losing weight if you're overweight
- getting more exercise (such as walking or swimming)
- moisturizing dry or cracked skin (but consult a doctor first)
Kabnick uses a pneumonic called the "6 Es" to help his patients remember these things: 1) elevation, 2) exercise, 3) emollient (moisturizer), 4) electrolytes (avoiding excess salt), 5) evaluation of lifestyle (avoid excess sitting/standing) and 6) enjoy the rest of your day (just for fun).
For more severe cases, medical intervention may be needed, Kabnick said. Today's treatments are minimally invasive, and most can be done in an outpatient clinic under local anesthesia.
Doctors will close up the larger veins that supply varicose veins using endovenous ablation. This can be done using one of three main types of procedures: endothermal (use of heat), endochemical (injection of chemicals) or endochemical-mechanical (use of chemicals and a hook-shaped tool), Kabnick said.
More serious problems with veins include deep veins thrombosis, blood clots deep in the circulatory system, which can be fatal, Kabnick said. In this case, medications and other techniques may be used to treat the condition and prevent it from becoming life threatening.
Follow Tanya Lewis on Twitter and Google+. Follow us @livescience, Facebook & Google+.

 Live Science Plus
Live Science Plus