New Drug May Ease Pain of Sickle Cell Anemia
A new drug may improve blood flow in patients with sickle-cell disease, easing pain and reducing their risk of dying from the condition, a new study suggests.
The drug is just one of many approaches being explored as a new therapy for sickle-cell disease. There is currently only one drug, called hydroxyurea, approved by the U.S. Food and Drug Administration to treat the condition, and not all patients respond to it.
"Hydroxyurea has been very useful, and for some patients, it's been terrific," said Dr. Martin Steinberg, a professor at Boston University School of Medicine who studies sickle-cell disease. But because it doesn't work for everyone, "it's vitally important to develop other types of medicine that work in ways that are different from how hydroxyurea works," he said.
The new study was conducted in mice, and further research is needed to determine if the drug will work in humans, the researchers said.The study was published Jan. 13 in the journal Blood.
Blocking blood vessels
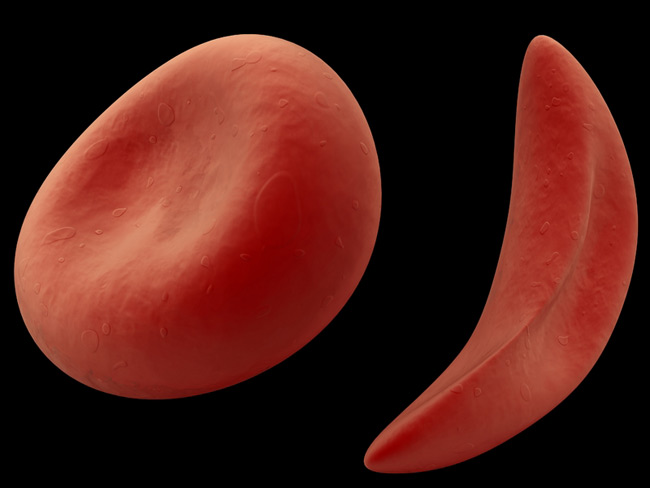
Sickle-cell disease is a hereditary condition in which red blood cells are a distorted shape they are sometimes C-shaped instead of their normal doughnut shape. The change stems from abnormal hemoglobin a protein in red blood cells that carries oxygen throughout the body. The cells can block blood vessels, leading to pain, organ and nerve damage and stroke. In a person with the condition, not all red blood cells are sickle-shaped all the time they take on the shape in response to a stressor, such as lack of oxygen, dehydration or infection.
People with sickle cell disease may have sickle cell anemia, the most severe form of the disease, or sickle cell trait, a less-severe form. In the United States, 70,000 to 100,000 African Americans are estimated to have sickle cell anemia, according to the Centers for Disease Control and Prevention.
Get the world’s most fascinating discoveries delivered straight to your inbox.
Researchers aren't entirely sure how the cells block blood vessels , but they seem to more easily stick to the inner lining of blood vessels. The new drug works by preventing sickle cells and white blood cells from adhering to the blood vessel walls.
The researchers injected the drug into mice, and then subjected the mice to a stressful situation an environment with low oxygen.The drug reduced the adhesion of the red blood cells to the blood vessel walls by 90 percent. The mice also showed increased blood flow and reduced mortality, compared with mice not injected with the drug.
The next step would be to test the drug in a clinical trial, said study researcher Diana Gutsaeva, a physiologist and molecular biologist at Georgia Health Sciences University in Atlanta.
A disadvantage of the therapy is it must be injected. A tablet form of the drug would be preferred because it is hard to get patients to comply with a treatment that must be injected, Steinberg said.
Another drug that works in a very similar way has already been tested in clinical trials, Steinberg said. However, the trial was stopped for financial reasons before the researchers could determine the drug's effectiveness.
Alternative avenues
Researchers don't know how hydroxyurea works, but they think it increases the amount of fetal hemoglobin in the body. Fetal hemoglobin is found in the red blood cells of fetuses and newborns, and has an enhanced ability to bind oxygen. It is also free from the abnormality that burdens sickle-cell hemoglobin. So red blood cells with fetal hemoglobin do not take on a sickle shape.
People lose their ability to make fetal hemoglobin a few months after birth. Hydroxyurea probably works by making it easier to make fetal hemoglobin again, Steinberg said.
Many new therapies for sickle-cell disease focus on trying to increase fetal hemoglobin in the body. For instance, some aim to turn on the genes that make fetal hemoglobin.
If the amount of fetal hemoglobin in the body could be increased so that 20 to 30 percent of red blood cells contain fetal hemoglobin instead of sickle hemoglobin and this was accomplished early in patients' lives the disease could be cured, Steinberg said.
In terms of future therapies, Steinberg said the most effective ones would probably increase fetal hemoglobin levels. But because this might not be possible, other avenues should be pursued, such as preventing cell adhesion. Other therapies involve giving patients nitric oxide , which relaxes blood vessels and has been shown to ease pain in sickle-cell patients.
"I think all these other things are potentially valuable adjuncts," Steinberg said. "They should all be pursued because you don't know what's going to come out at the end," he said.
Pass it on: A new drug that prevents sickle cells from sticking to blood vessel walls may one day provide an alternative therapy for sickle-cell disease. Researchers are currently investigating many new treatment paths as there is only one approved drug for the condition.
- What Is Sickle Cell Disease?
- Adults Struggle with What Used to Be Child's Blood Disorder
- Squishy Particles Could Become New Type of Artificial Blood
Follow MyHealthNewsDaily staff writer Rachael Rettner on Twitter @Rachael_MHND.

Rachael is a Live Science contributor, and was a former channel editor and senior writer for Live Science between 2010 and 2022. She has a master's degree in journalism from New York University's Science, Health and Environmental Reporting Program. She also holds a B.S. in molecular biology and an M.S. in biology from the University of California, San Diego. Her work has appeared in Scienceline, The Washington Post and Scientific American.
 Live Science Plus
Live Science Plus





