Pancreatitis: Causes, symptoms and treatments
Pancreatitis, or inflammation of the pancreas, can occur in a chronic or acute form.

Get the world’s most fascinating discoveries delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?

Delivered Daily
Daily Newsletter
Sign up for the latest discoveries, groundbreaking research and fascinating breakthroughs that impact you and the wider world direct to your inbox.

Once a week
Life's Little Mysteries
Feed your curiosity with an exclusive mystery every week, solved with science and delivered direct to your inbox before it's seen anywhere else.

Once a week
How It Works
Sign up to our free science & technology newsletter for your weekly fix of fascinating articles, quick quizzes, amazing images, and more

Delivered daily
Space.com Newsletter
Breaking space news, the latest updates on rocket launches, skywatching events and more!

Once a month
Watch This Space
Sign up to our monthly entertainment newsletter to keep up with all our coverage of the latest sci-fi and space movies, tv shows, games and books.

Once a week
Night Sky This Week
Discover this week's must-see night sky events, moon phases, and stunning astrophotos. Sign up for our skywatching newsletter and explore the universe with us!
Join the club
Get full access to premium articles, exclusive features and a growing list of member rewards.
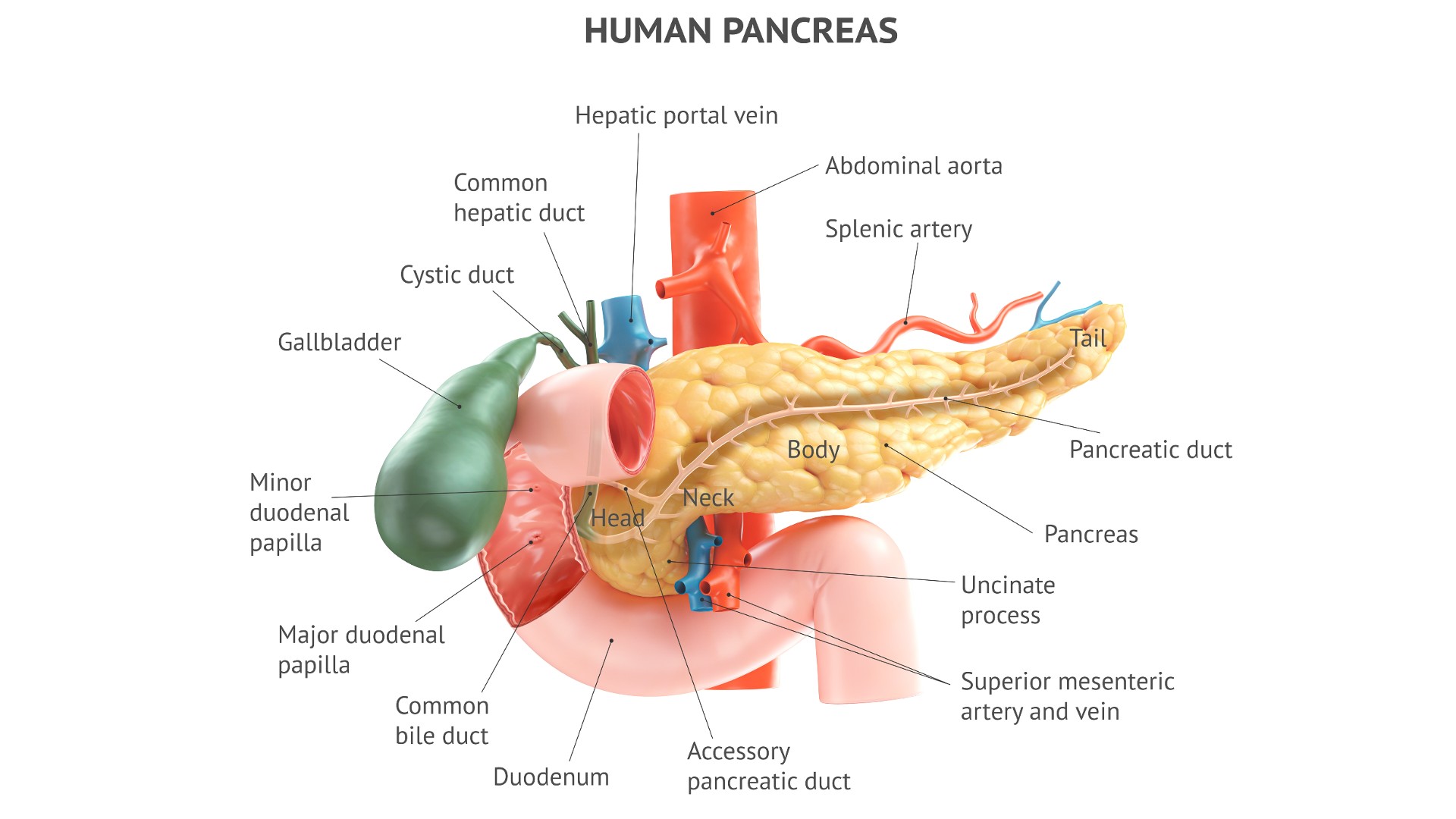
Pancreatitis refers to inflammation of the pancreas, an organ located in the back of the upper abdomen, behind the stomach, that secretes hormones and digestive juices.
The condition can occur as a short-term, severe condition called acute pancreatitis. Alternatively, it can occur as a long-term disease that waxes and wanes, called chronic pancreatitis.
What causes pancreatitis?
The pancreas can become inflamed for a variety of reasons. The two most common reasons are gallstones — pebble-like masses that form in the gallbladder or ducts between the liver and small intestine — and alcohol misuse. To understand what causes pancreatitis, it's important to know what the pancreas does and how it is structured.
Located in the upper abdomen, behind the stomach, the pancreas is both an endocrine gland (a gland that secretes hormones into the bloodstream) and an exocrine gland (a gland that secretes substances, such as enzymes, through ducts and/or to the body's surface), according to Columbia Surgery. Whereas the pancreas makes and secretes four hormones as its endocrine function, its exocrine function is to make, store and secrete a variety of enzymes needed for the digestion of nutrients from food.
Pancreatic digestive enzymes are made in "acinar cells" and are secreted into a network of ducts that ultimately feeds into the main pancreatic duct. The main pancreatic duct carries pancreatic enzymes to the first part of the small intestine, called the duodenum. However, prior to reaching the duodenum, the pancreatic duct merges with another duct, called the common bile duct, which carries a substance called bile from the liver and gallbladder. It's common for gallstones to block the common bile duct. This can prevent pancreatic secretions from moving from the main pancreatic duct into the duodenum, and this backup can lead to inflammation of the pancreas, or pancreatitis.
The digestive enzymes made by acinar cells start out as zymogens — inactive precursors to the enzymes that are stored in protective bubbles known as vesicles. These zymogens can only be "activated" by other enzymes in the cell, whose activity are kept in check by still other enzymes. Alcohol disrupts the balance of all of these enzymes, causing the system of enzymes to shift in favor of more digestive enzymes being activated and released from acinar cells. This causes inflammation in the pancreas, which is why alcohol misuse can cause pancreatitis.
In addition to gallstones and alcohol misuse, other causes of pancreatitis include high levels of serum triglycerides (fat molecules in the blood); certain viral infections, including mumps; or trauma to the pancreas. Rarely, the condition may be tied to the use of certain medications, including steroids, or exposure to toxins, such as scorpion venom. Finally, some cases of pancreatitis are called idiopathic, meaning there is no identifiable cause.
Get the world’s most fascinating discoveries delivered straight to your inbox.
As noted above, pancreatitis can be acute, meaning it develops over hours to days and requires immediate attention, or chronic, meaning it waxes and wanes in milder episodes. The causes mentioned above can result in both acute and chronic pancreatitis, since the chronic condition can develop as a result of a person having multiple episodes of acute pancreatitis. These episodes make the pancreatic tissue increasingly susceptible to inflammation.
Alcohol misuse can cause chronic pancreatitis, even without causing acute pancreatitis along the way. In addition, autoimmune diseases, in which the immune system attacks the body's tissues, can cause chronic pancreatitis.
Pancreatitis risk factors
As noted above, the pancreas can become inflamed for a variety of reasons, the most common being alcohol misuse and gallstones. Factors linked to an increased risk of gallstones, and thus an increased risk of pancreatitis, include the following:
- Being overweight or obese
- Being over age 40
- Being of Hispanic or Native American heritage
- Being female
- Having had multiple pregnancies
What are the symptoms of pancreatitis?
Symptoms of pancreatitis include:
- Pain just below the ribs, which typically radiates around your torso to the back in a belt-shaped pattern. The pain tends to worsen after a meal, because the meal stimulates the secretion of pancreatic enzymes.
- Nausea and vomiting
- Chills and/or fever
- Heart palpitations, which are suggestive of a rapid heartbeat
- Abdominal swelling
How is pancreatitis diagnosed?
Doctors will evaluate a patient's symptoms and medical history, as well as check for signs of pancreatitis that may appear on physical examination, such as jaundice (yellowing of the skin and eyes), rapid heartbeat and abdominal swelling.
Doctors will order blood samples for various lab tests, such as a comprehensive metabolic panel (CMP), a complete blood count (CBC) and often liver function tests. Particularly important information comes from tests for levels of enzymes called lipase and amylase, which are pancreatic enzymes that leak into the blood when the pancreas is inflamed. A finding that lipase and amylase levels are elevated at least three times the upper limit of the normal range suggests acute pancreatitis. Of these two enzymes, lipase is more specific than amylase for pancreatitis, meaning that amylase is often elevated due to causes other than pancreatitis.
Oftentimes, these enzyme levels are not as elevated in cases of chronic pancreatitis, because the episodes of inflammation tend to be milder.
Doctors can obtain a clear diagnosis of acute or chronic pancreatitis by way of specialized imaging tests that can be used to reveal changes in the pancreas that are indicative of each condition. One of the tests is called cholangiopancreatography (ERCP), and the other is called magnetic resonance cholangiopancreatography (MRCP).
In addition to its diagnostic capability, ERCP offers the advantage of being able to treat some causes of pancreatitis — for instance, by removing a gallstone. However, ERCP also has disadvantages. For example, it can actually cause an episode of acute pancreatitis if contrast dye is inadvertently injected into the pancreatic tissue itself, instead of into the ducts that it is supposed to help image.
Complications of pancreatitis
Both acute and chronic pancreatitis can cause digestive problems, such as diarrhea and inadequate absorption of food and of the kind of vitamins that dissolve in fat. This means that pancreatitis can lead to nutritional deficiencies and weight loss.
Because episodes of acute pancreatitis can lead to chronic pancreatitis, chronic pancreatitis would be considered a complication of the acute condition. Other complications of acute pancreatitis include bleeding in the pancreas, kidney failure, and infection leading to pancreatic necrosis, meaning the death of pancreatic tissue. Additionally, infection and necrosis of the pancreas can lead to sepsis, a life-threatening, body-wide immune reaction. In pregnancy, acute pancreatitis can trigger preterm birth or potentially cause fetal death.
Complications of chronic pancreatitis can include abdominal pain that comes and goes; depression and anxiety; and diabetes, due to destruction of pancreatic beta cells, which produce the hormone insulin. Chronic pancreatitis is also linked to an increased risk of pancreatic cancer.
How is pancreatitis treated?
In evaluating a case of pancreatitis, doctors consider the patient's age and various lab test results together, using what doctors call the Ranson criteria.
The Ranson criteria generate a score that is used to determine whether the pancreatitis is mild or likely to be severe acute pancreatitis. If it's mild, that would require only monitoring and supportive measures, meaning that the patient would be admitted to the hospital and hydrated with intravenous fluids, with no food allowed.
In the case of severe acute pancreatitis, the patient must be admitted to the intensive care unit, as there could be dangerous complications, including bleeding in the pancreas, infection, necrosis and sepsis.
Acute pancreatitis with bacterial infection requires treatment with antibiotics, according to the 2019 World Journal of Emergency Surgery guidelines for the management of severe acute pancreatitis. Other potential medical treatments include supplemental digestive enzymes to replace enzymes that the pancreas fails to produce; pain medication; or corticosteroids for autoimmune-driven pancreatitis.
This article is for informational purposes only and is not meant to offer medical advice.
David Warmflash is a medical researcher, astrobiologist, science communicator, and author, located in Portland, Oregon. He holds an MD from Tel Aviv University Sackler School of Medicine and has conducted research in astrobiology, space biology, and space medicine during research fellowships at NASA's Johnson Space Center, the University of Pennsylvania, and Brandeis University, and in collaboration with The Planetary Society and the Israeli Aerospace Medicine Institute.
 Live Science Plus
Live Science Plus