
Epidemic: Killer TB Spreads As Research Plummets (Op-Ed)
Get the world’s most fascinating discoveries delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?
Join the club
Get full access to premium articles, exclusive features and a growing list of member rewards.
Colleen Daniels, director for TB and HIV at the Treatment Action Group, contributed this article to Live Science's Expert Voices: Op-Ed & Insights.
In a recent Huffington Post article, Francis Collins, director of the U.S. National Institutes of Health, said that the nation would most likely have a vaccine and therapeutics for Ebola if investment had not stagnated. Substitute the word Ebola for tuberculosis (TB) and you can accurately describe the situation facing TB today.
Globally, more than 8 million people get sick, and 1.3 million die, from TB each year — in 2013, there were 9,582 TB cases and 10 million people living with TB infection in the United States.
Antibiotic research has collapsed
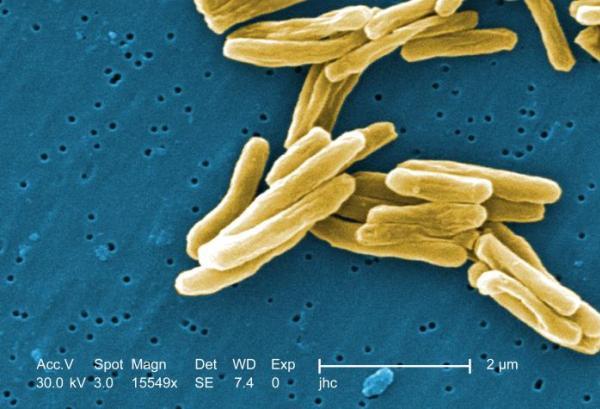
Tuberculosis is a preventable and curable disease caused by the Mycobacterium tuberculosis bacteria. Transmitted through the air, it most often affects the lungs — and the medical community is not even close to eliminating it. Rising cases of drug-resistant TB, high mortality for people with both HIV and TB, and an environment of continued funding cuts for research and development means that communities dealing with the disease are on a potentially devastating trajectory. Pharmaceutical companies are leaving the anti-infectives field in droves because they are all searching for the next blockbuster drug that will bring in billions of dollars — those companies do not see antibiotics as having a good return on investment. However, with one third of the world's population having latent TB infection, one might think there would be a good market incentive.
Ebola and TB are not the only diseases facing a lack of investment in research and development — annually across the globe, dengue affects 50 million to 100 million people, Chagas affects 15 million, and the leishmaniases affect 12 million annually. [2014 Ebola Outbreak: Full Coverage of the Viral Epidemic ]
Pfizer, AstraZeneca and Novartis all closed the door on all antibiotic development in the last two years. Their departure comes at a time when their investment is needed most, with urgent calls for new drugs to treat rising drug resistance for diseases like TB.
Get the world’s most fascinating discoveries delivered straight to your inbox.
U.S. President Barack Obama's executive order combatting antibiotic resistance and accompanying National Strategy for Combatting Antibiotic Resistant Bacteria categorize drug-resistant tuberculosis as a serious threat-level pathogen. And, the U.S. Centers for Disease Control and Prevention (CDC)'s report, "Antibiotic Resistance Threats in the United States, 2013," listed TB as Hazard Level: Serious. The CDC categorized drug-resistant pathogens as urgent, serious and concerning. (Hazard levels were determined by criteria such as clinical and economic impact, incidence, availability of effective antibiotics and transmissibility.)
Despite those alarming warnings, TB is still not a priority research area for pharmaceutical companies, the U.S. government, or any other government. The president's executive order recommended funding of $900 million per year for antibiotic research and an additional $800 million per year as an incentive for pharmaceutical industry involvement. Those funds remain "suggested," but uncommitted.
Combatting an epidemic
The "Global Plan to Stop TB 2011-2015" calls for an annual investment of $2 billion to develop the new drugs, diagnostics and vaccines needed to end the global TB epidemic. In 2013, the world spent $676.6 million on such development — that's just 33 percent of the annual amount needed, according to an analysis Treatment Action Group conducted. Now in its ninth year, our 2014 "Report on Tuberculosis Research Funding Trends" shows that the foundation of the TB research enterprise is shakier than ever, setting back efforts to fight the disease.
In 2013, private sector companies spent $99.6 million on TB research, a 31.32 percent decline from the $144.97 million that industry invested in 2011. With investments now under $100 million, pharmaceutical companies spent less on TB research and development (R&D) in 2013 than they did in 2009, at the peak of the global economic crisis.
Just one company — Otsuka (Tokyo, Japan) — accounts for 60 percent of all private-sector spending on TB R&D.
Low levels of investment have produced research of poor quality and little volume. In the last 40 years, only two new drugs from new drug classes have been approved to treat TB. Phase I of the TB drug pipeline sits empty, guaranteeing that the existing drugs will not be followed by other new compounds for years to come.
"When companies pull out of TB research, we not only lose their financial capital, but promising compounds owned by these companies get stuck in early stages of development. As a result, the pace of research is falling behind the spread of drug-resistant TB," said Mark Harrington, executive director of TAG.
Stopping TB before it's too late
TB research relies heavily on a small number of funders, mostly public and philanthropic institutions. In 2013, the 20 largest funders of TB R&D gave almost 90 percent of the total $676.3 million. The two largest donors — the U.S. National Institute of Allergy and Infectious Diseases (NIAID) and the Bill & Melinda Gates Foundation — together gave 45 percent of all money spent on TB research in 2013.
The public sector gives four times more money to TB R&D than private industry, and philanthropic institutions give twice as much.
Torpid funding for TB R&D means that the pace of research is now falling far behind the spread of drug-resistant TB. In 2012, the World Health Organization estimated that 450,000 people developed multidrug-resistant TB, yet only 1 in 6 of them started treatment.
Today, we continue to use diagnostics that are 120 years old, are inaccurate and do not work on children or people with HIV. We still give treatment regimens that are lengthy (from 6-24 months), highly toxic — which can cause side effects such as psychosis and deafness — and only cure about half of patients with multidrug-resistant TB.
Those who get sick surely deserve better options than having to choose between keeping their hearing or a chance at curing their TB. The current R&D model is broken and failing TB patients.
Initiatives to support antibiotic research — of which TB drug and diagnostic R&D are crucial parts — must be backed by funding commensurate to the growing size of the epidemic.
Follow all of the Expert Voices issues and debates — and become part of the discussion — on Facebook, Twitter and Google+. The views expressed are those of the author and do not necessarily reflect the views of the publisher. This version of the article was originally published on Live Science.
 Live Science Plus
Live Science Plus











