Osteoarthritis: Causes, Symptoms & Treatment

Get the world’s most fascinating discoveries delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?
Join the club
Get full access to premium articles, exclusive features and a growing list of member rewards.
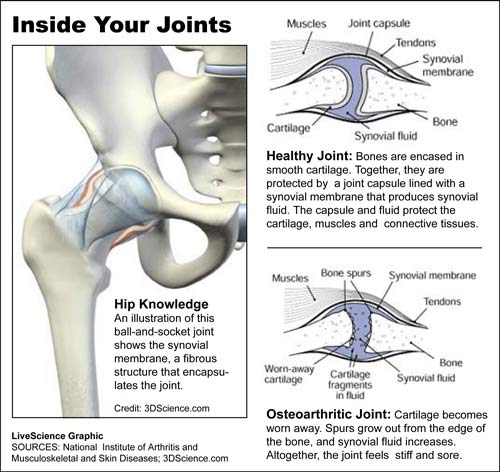
Osteoarthritis, also known as degenerative joint disease, occurs when cartilage between the joints wears down over time, which can cause pain, loss of motion, swelling and joint stiffness. The most commonly affected joints are the knees, hips, neck, tips of the fingers, thumbs and lower back.
Without cartilage between the bones at the joint, the bones rub together painfully, and the joint may even warp from its normal shape. Small bone spurs can grow on the edges of the joint, which can cause discomfort, reports The National Institute of Arthritis and Musculoskeletal and Skin Diseases. Pieces of bone or cartilage can also break away and float inside the joint, leading to additional pain and problems.
Osteoarthritis is the most common form of arthritis. The disease progresses gradually, and usually does not begin until after age 40.
Causes
Cartilage on the ends of your bones helps absorb the shock of movement. But when cartilage is damaged or breaks down, this "cushion" degrades. Cartilage damage can be caused by a direct blow, such as kick or fall; wear and tear over a prolonged period; and lack of movement over a prolonged period, reports Medical News Today.
Risk factors for osteoarthritis (sometimes spelled "osteoarthrosis") include being overweight, getting older, and experiencing joint injuries, according to the National Institutes of Health. Osteoarthritis in the hands is hereditary and also most common in postmenopausal women.
Symptoms
Symptoms of osteoarthritis include: pain, swelling, stiffness and reduced motion in the joints. People with osteoarthritis may also experience a "crunching" feeling, which is the joints rubbing together. Some people even hear the sound of bone scraping against bone. Osteoarthritis is not usually accompanied by red or hot skin, rashes, or fevers, so if you experience those symptoms, you may have another health condition.
Different people experience osteoarthritis in different ways, reports The National Institute of Arthritis and Musculoskeletal and Skin Diseases. For some, it progresses quickly; for the majority, however, it develops slowly over the years. Early on, joints may feel stiff or sore after exercise, but as the problem progresses the pain may become prolonged and more intense. It is more typical to feel stiff upon first waking up or after sitting still for a long time.
Get the world’s most fascinating discoveries delivered straight to your inbox.
In addition to stiffness and pain, those suffering from osteoarthritis in the hands may experience small, bony knobs growing at the ends or middles of the fingers. Fingers can also become enlarged, gnarled or numb. Those with osteoarthritis in the spine (typically at the lower back or neck) may feel weakness, numbness, or tingling in the arms and legs. This is caused by the spine, swollen or stiff from osteoarthritis, putting new pressure on the nerves.
People who have questions about osteoarthritis or who experience joint pain or stiffness that lasts for more than a few weeks should see a doctor.
Treatment
There is no cure for osteoarthritis, according to the Centers for Disease Control, so treatment focuses on relieving symptoms and improving joint function. A doctor can help determine treatment options.
In March 2014, the Osteoarthritis Research Society International (OARSI) released new guidelines for non-surgical treatment of osteoarthritis. The non-profit research group's goal was to help health care providers determine which therapies would be most useful for individual patients. After researching existing literature, an OARSI committee condensed its findings into 25 treatment recommendations, which are listed on the Arthritis Foundation's website. The recommendations are:
1. Drug and non-drug treatments (The optimal treatment program should consist of both medications and non-drug treatments.)
Non-drug treatments
2. Education and self-management
3. Regular telephone contact with a layperson to promote self-care
4. Physical therapy
5. Aerobic, muscle-strengthening and water-based exercises
6. Weight loss
7. Walking aids (Canes, crutches, wheeled walkers)
8. Footwear and insoles
9. Knee braces
10. Heat and cold (warm bath, heat pack or paraffin bath; cold packs)
11. Transcutaneous electrical nerve stimulation (TENS) — A technique in which a weak electric current is administered through electrodes placed on the skin. It is thought to work by stopping messages from pain receptors from reaching the brain. It has been shown to help with short-term pain control in some patients with knee or hip arthritis.
12. Acupuncture
Drug treatments
13. Acetaminophen
14. Nonsteroidal anti-inflammatory drugs (NSAIDs)
15. Topical analgesics (NSAIDs and Capsaicin)
16. Corticosteroid injections
17. Hyalruonic acid injections
18. Glucosamine and/or chondroitin for symptom relief
19. Glucosamine sulfate, chondroitin and/or diacerein for possible structure-modifying effects
20. Opioid and narcotic analgesics
Surgery
21. Joint replacement surgery
22. Unicompartmental (partial) knee replacement
23. Osteotomy and joint-preserving surgery
24. Joint lavage and arthroscopic debridement
25. Joint fusion when replacement has failed
Jessie Szalay contributed to this article.

Rachael is a Live Science contributor, and was a former channel editor and senior writer for Live Science between 2010 and 2022. She has a master's degree in journalism from New York University's Science, Health and Environmental Reporting Program. She also holds a B.S. in molecular biology and an M.S. in biology from the University of California, San Diego. Her work has appeared in Scienceline, The Washington Post and Scientific American.
 Live Science Plus
Live Science Plus