Baby Farms of the Future? Docs Warn of Ethical Issues from New Tech
Get the world’s most fascinating discoveries delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?

Delivered Daily
Daily Newsletter
Sign up for the latest discoveries, groundbreaking research and fascinating breakthroughs that impact you and the wider world direct to your inbox.

Once a week
Life's Little Mysteries
Feed your curiosity with an exclusive mystery every week, solved with science and delivered direct to your inbox before it's seen anywhere else.

Once a week
How It Works
Sign up to our free science & technology newsletter for your weekly fix of fascinating articles, quick quizzes, amazing images, and more

Delivered daily
Space.com Newsletter
Breaking space news, the latest updates on rocket launches, skywatching events and more!

Once a month
Watch This Space
Sign up to our monthly entertainment newsletter to keep up with all our coverage of the latest sci-fi and space movies, tv shows, games and books.

Once a week
Night Sky This Week
Discover this week's must-see night sky events, moon phases, and stunning astrophotos. Sign up for our skywatching newsletter and explore the universe with us!
Join the club
Get full access to premium articles, exclusive features and a growing list of member rewards.
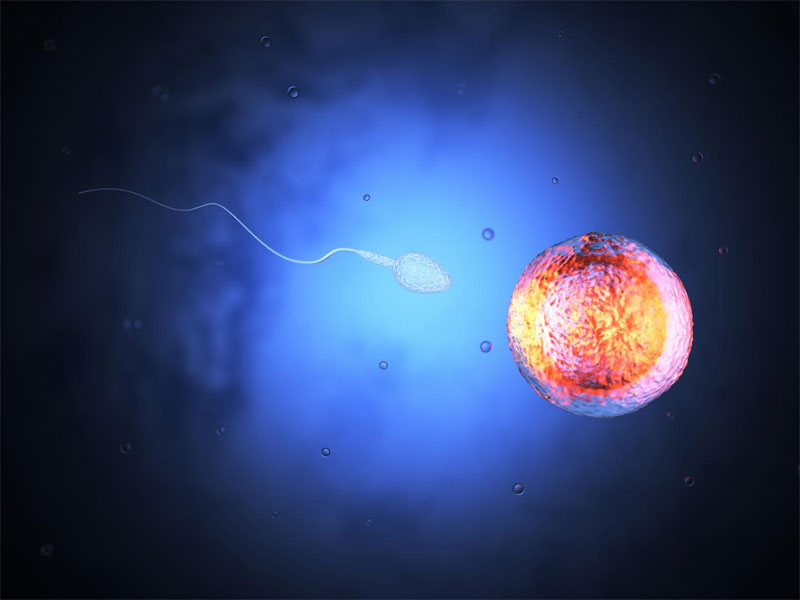
In the not-too-distant future, scientists may be able to create human sperm and egg cells in a lab dish. That possibility brings hope for treating infertility, but also poses significant ethical dilemmas — from "embryo farming" to designer babies, some researchers argue.
In a new paper, researchers at Harvard and Brown universities discuss the theoretical implications of creating sperm and egg cells in a lab dish, referred to as "in vitro gametogenesis," or IVG. It's currently feasible to perform IVG in mice, as has been shown in several remarkable experiments that were published in recent years, said the paper's authors, Dr. Eli Adashi, a professor of medical science at Brown University in Providence, Rhode Island; I. Glenn Cohen, a professor at Harvard Law School in Boston; and Dr. George Daley, dean of Harvard Medical School also in Boston.
IVG is not yet possible in humans — just from a scientific standpoint, many technical barriers remain before human gametes could be made from other human cells, the authors said. Even so, the technology could arrive sooner than we think, and so it may be wise to ponder some of the regulatory and ethical questions raised by IVG now, they said. [Conception Misconceptions: 7 Fertility Myths Debunked]
"With science and medicine hurtling forward at breakneck speed, the rapid transformation of reproductive and regenerative medicine may surprise us," the authors wrote in their paper, which was published today (Jan. 11) in the journal Science Translational Medicine. "Before the inevitable, society will be well advised to strike and maintain a vigorous public conversation on the ethical challenges of IVG."
What is IVG?
IVG is the generation of sperm and egg cells in a lab dish from pluripotent stem cells, or cells that are capable of becoming any cell type in the body, the paper said. These could be embryonic stem cells, which are found in embryos during early stages of development, or so-called induced pluripotent stem cells (iPS cells), which are "adult" cells (such as skin cells) that have been reprogrammed so they are once again capable of becoming any cell type. Hypothetically, IVG could create human sperm and egg cells from adult skin cells.
Scientists have recently reported key successes with IVG in mice. In 2016, scientists in Japan reported that they could recreate the entire cycle of mouse egg production in a lab dish. They started with either embryonic stem cells or iPS cells from mice, and reprogrammed them into so-called primordial germ cells, which are the precursors of sperm or egg cells. Then, they mixed these cells with other cells that support the development of mouse eggs, creating a sort of ovary in a dish. They added various hormones and other compounds to the dish, and eventually found a way to coax the cells into developing properly to become egg cells. These egg cells were fertilized with sperm, and resulted in healthy baby mice pups.
Get the world’s most fascinating discoveries delivered straight to your inbox.
Also in 2016, researchers in China said that they had created sperm-like cells from embryonic stem cells that were taken from mice. For these experiments, the researchers first turned embryonic stem cells into primordial germ cells and then cultured these cells with testosterone and other hormones, which prompted the cells to develop into immature sperm cells.
Other studies suggest that similar feats with human cells might be possible. In 2009, researchers at Stanford University reported that they had transformed human embryonic stem cells into germ cells, which could theoretically give rise to sperm and eggs (although the researchers did not let the cells develop for long enough to become sperm or eggs).
"These findings suggest that experimental refinements likely will permit derivation of functional eggs and sperm from [human stem cells] in the not too distant future," Adashi, Cohen and Daley wrote in their paper.
IVG in people
In people, IVG could revolutionize the way that doctors perform in vitro fertilization (IVF) to treat infertility, Adashi, Cohen and Daley said. Currently, women who have fertility problems may undergo IVF, which involves several weeks of hormone injections to stimulate the production of eggs, and then a procedure to retrieve the eggs, which is done at a doctor's office. IVG would eliminate the need for these steps and would also eliminate the need to find an egg donor if a woman couldn't use her own eggs, they said.
What's more, with an abundant source of egg and sperm cells, researchers could more easily study the process of embryonic development and certain diseases, they said.
But IVG could also lead to new ethical problems. For example, clinics might create scores of eggs or embryos for their clients. "IVG may raise the specter of 'embryo farming' on a scale currently unimagined, which might exacerbate concerns about the devaluation of human life," they said.
In addition, couples might create a large number of embryos in order to choose the best traits for their child. (Currently, IVF usually generates just a handful of embryos, which doctors can screened for certain diseases before choosing which ones to implant..) "IVG could, depending on its ultimate financial cost, greatly increase the number of embryos from which to select, thus exacerbating concerns about parents selecting for their 'ideal' future child," they said.
IVG might even one day allow people to create "single-parent babies," in which cells from one person are used to produce both sperm and egg. However, it's not yet clear whether cells from a male can produce eggs (and vice versa), or whether a baby with just a single parent would have the same health problems that can arise from having closely related parents, they said. [Controversial Human Embryo Editing: 5 Things to Know]
Finally, it might also be possible for people to become parents without their knowledge, if sperm and egg cells could be created from shed skin cells, they said.
Still, in the near future, the biggest impact of IVG will likely be to enhance the scientific understanding of reproductive cells, the researchers said. Any applications of it could be much further out.
The authors note that some of the concerning scenarios raised in their paper would require a deeper understanding of human genetics than we currently have in order to be made possible. "Nevertheless, even at this stage, it is worth contemplating the ethical issues raised by such a possible future," they said.
Original article on Live Science.

Rachael is a Live Science contributor, and was a former channel editor and senior writer for Live Science between 2010 and 2022. She has a master's degree in journalism from New York University's Science, Health and Environmental Reporting Program. She also holds a B.S. in molecular biology and an M.S. in biology from the University of California, San Diego. Her work has appeared in Scienceline, The Washington Post and Scientific American.
 Live Science Plus
Live Science Plus