Insulin resistance: Risk factor for heart disease and diabetes
Insulin resistance is a condition where the body's cells don't properly respond to the hormone insulin.

Insulin resistance is a condition in which the hormone insulin, which regulates blood sugar levels, is unable to do its job.
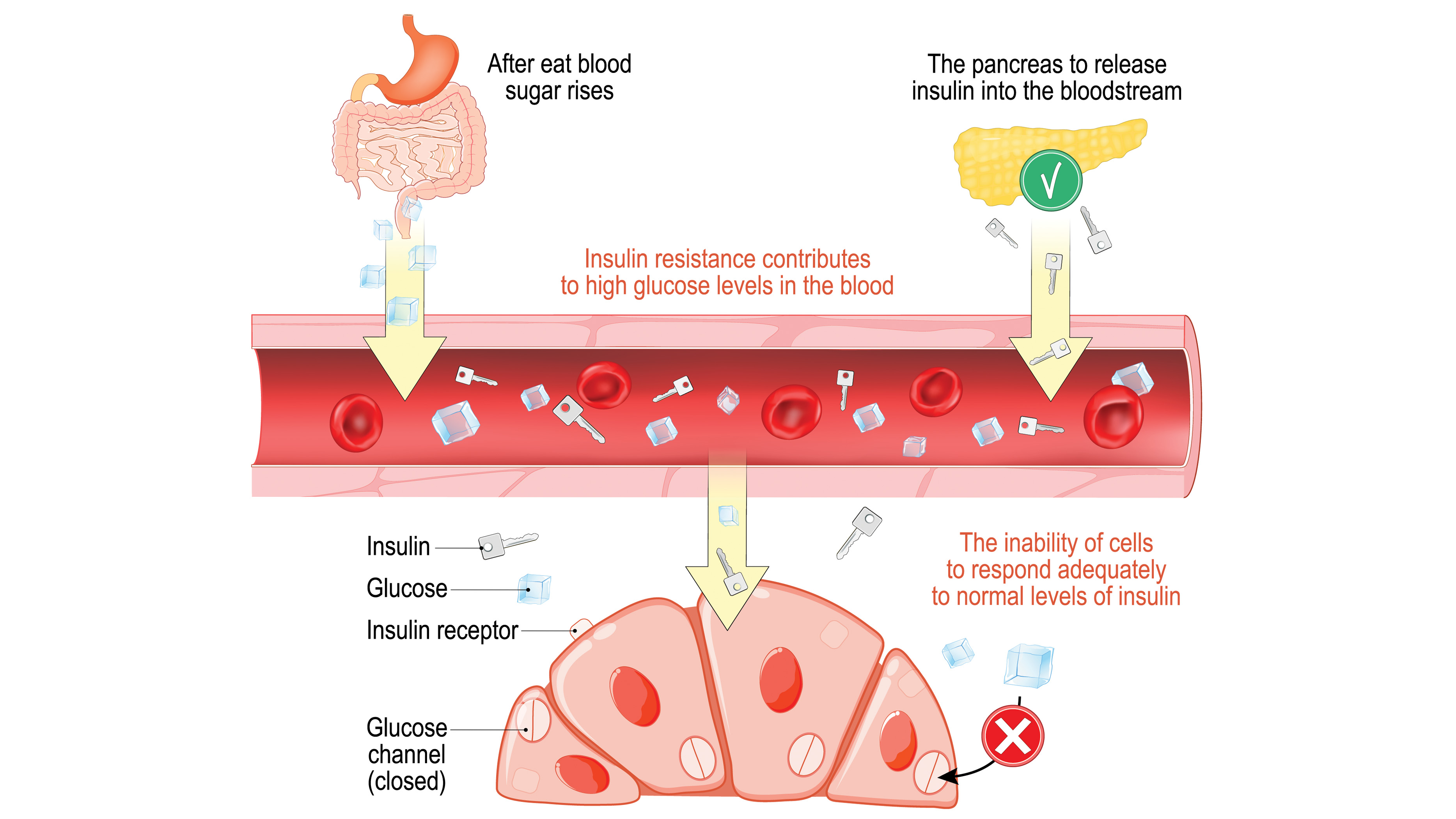
Under normal circumstances, glucose (or sugar) enters the bloodstream after the body breaks down food that has been consumed. The pancreas secretes insulin to help glucose (the body's main source of energy) enter muscle, fat and liver cells so the glucose can be used for energy or stored for later use.
But when a person has insulin resistance, this process goes awry.
"Think of insulin as the key that unlocks the door to their cells. That door needs to be opened in order for glucose to exit the blood into the cell," said Kimber Stanhope, a nutrition research scientist at the University of California at Davis.
When people are insulin resistant, their pancreas is still making those "keys," but they don't work so well to unlock cells and let in glucose, Stanhope said.
Related: What is normal blood sugar?
In the early stages of insulin resistance, cells start to ignore the signal from insulin to take in glucose from the blood. So the pancreas pumps out more insulin to shepherd glucose into cells and blood sugar mostly stays at a normal level. But over time, the cells stop responding even to those higher levels of insulin.
Get the world’s most fascinating discoveries delivered straight to your inbox.
"It's not like you suddenly don't respond to insulin," said Calum Sutherland, a professor of molecular and cellular diabetes at the University of Dundee in the U.K. "Maybe in the initial stages, you drop 10% of your response, and then after a few months it may drop 30%, and after a few years it may drop 60%. And so, progressively your body loses its ability to respond appropriately to insulin."
Eventually, the pancreas can't keep up, and blood sugar levels rise.
People with persistently elevated blood sugar are diagnosed with either prediabetes (in which blood sugar levels are high but not high enough to meet the benchmark for diabetes) or type 2 diabetes, which can lead to a host of life-threatening complications if left untreated, according to the CDC. In 2019, about 96 million U.S. adults had prediabetes, according to data from the Centers for Disease Control and Prevention. (CDC)
Causes of insulin resistance
It's not totally clear what causes insulin resistance, according to the American Diabetes Association (ADA).
However, several risk factors have been linked with insulin resistance, including being overweight or obese and having a family history of type 2 diabetes, according to the CDC.
Some researchers suspect that extra fat tissue may cause inflammation, physiological stress or other changes that contribute to insulin resistance, according to the ADA.
(Separately, insulin resistance also contributes to weight gain, leading to a vicious cycle.)
Although being overweight is a risk factor for insulin resistance and diabetes, some people with insulin resistance or diabetes are not overweight. In fact, about 10% to 15% of people with type 2 diabetes are at a healthy weight, according to WebMD.
Inactivity is also a risk factor for insulin resistance, according to the National Diabetes Information Clearinghouse. Inactivity may lead to insulin resistance because muscle tissue uses more glucose than other types of tissue, and muscle becomes better at taking up sugar after exercise. People who exercise infrequently do not benefit from this effect.
Aging is also tied to insulin resistance, because people typically lose muscle mass as they age, according to a 2021 review article in the journal Comprehensive Physiology. Lower muscle mass means fewer cells that can take in large amounts of glucose.
Symptoms and diagnosis
Most people in the early stages of insulin resistance have no symptoms and no idea that they are on the pathway to disease. And doctors do not diagnose insulin resistance — also referred to as impaired insulin sensitivity — it is usually only measured in research studies.
"We don't have a threshold where we say someone is insulin resistant," Sutherland told Live Science.
Doctors may instead diagnose a related condition known as metabolic syndrome, which includes high blood sugar, high cholesterol and high blood pressure levels and excess belly fat, according to the National Heart, Lung and Blood Institute.
Many people only find out about their blood sugar-processing problems when they start showing symptoms of prediabetes and type 2 diabetes, which is a lifelong, progressive condition. These symptoms include increased thirst, hunger and urination, blurred vision, and slow healing of cuts and sores, according to the Cleveland Clinic.
To diagnose high blood sugar, doctors may order an A1C blood test, which measures a person's average blood glucose over the preceding three months, or the fasting plasma glucose test, which reveals how effectively the body metabolizes glucose after a person has fasted for eight hours.
Doctors may also order tests that help to diagnose other conditions associated with insulin resistance, such as cardiovascular disease and polycystic ovary syndrome (PCOS), which is a hormonal disorder that can affect women of reproductive age, according to the Cleveland Clinic.
Insulin resistance and diet
Insulin resistance is common nowadays in part because of our Western diets, Sutherland told Live Science. (Western diets are typically high in calories, refined grains and ultraprocessed foods and low in fiber.)
Although no single diet has shown to be most effective, certain diets may improve insulin sensitivity. For instance, diets low in simple or processed sugars but high in fiber and complex carbohydrates may be helpful, according to a review study published in 2019 in the journal Advances in Clinical and Experimental Medicine.
The Mediterranean diet — which emphasizes eating vegetables and fruits, nuts, whole grains, fish and extra virgin olive oil— has been shown in several studies to reduce insulin resistance.
And the Dietary Interventions to Stop Hypertension (DASH) diet — which emphasizes vegetables and fruits, low-fat dairy foods and limits sweets, salt and saturated fats — has also been associated with lower insulin resistance, several studies show.
Can insulin resistance be reversed?
In some people, insulin resistance can be reversed, said Richard Mackenzie, a researcher who studies insulin resistance and metabolism at the University of Roehampton in the U.K.
"We know with weight/fat loss that insulin resistance improves," Mackenzie told Live Science in an email. "We know that gastric bypass surgery [a type of weight loss surgery] can completely reverse insulin resistance in the matter of days."
To aid such weight loss, doctors may recommend eating fewer processed carbohydrates and less unhealthy fat, sugar, red meat and processed starches, according to the Cleveland Clinic.
The Diabetes Prevention Program, a long-running study funded by the National Institutes of Health, found that for people at high risk of developing diabetes, losing 5% to 7% of their starting weight helped reduce their chances of developing the disease. (Participants in the study lost weight by changing their diet and being more physically active.)
Physical activity — both high-intensity interval training and moderate physical activity — also increases glucose energy usage and improves muscle insulin sensitivity, a clinical trial published in 2020 found.
Some people with insulin resistance may benefit from a drug called metformin, which reduces the amount of glucose the liver makes and prompts the muscles and other tissues to take up more blood sugar. The results of the Diabetes Prevention Program showed that metformin worked best for younger adults, people with obesity and people with a history of gestational diabetes.
This article is for informational purposes only and is not meant to offer medical advice.
This article was updated on Feb. 8, 2022, by Live Science contributor Natalie Grover.
Additional resources
- Check out this report by Yale on the latest research linking insulin resistance to fatty liver disease.
- Learn more about metformin in this review published by the Mayo Clinic.
Bibliography
American Diabetes Association. Understanding insulin resistance. https://www.diabetes.org/healthy-living/medication-treatments/insulin-resistance
Centers for Disease Control and Prevention. Insulin resistance and diabetes.
https://www.cdc.gov/diabetes/basics/insulin-resistance.html
Cleveland Clinic. Insulin resistance. https://my.clevelandclinic.org/health/diseases/22206-insulin-resistance
National Institute of Diabetes and Digestive and Kidney Diseases. Diabetes Prevention Program (DPP). U.S. Department of Health and Human Services, National Institutes of Health. https://www.niddk.nih.gov/about-niddk/research-areas/diabetes/diabetes-prevention-program-dpp
National Institute of Diabetes and Digestive and Kidney Diseases.Insulin resistance & prediabetes. U.S. Department of Health and Human Services, National Institutes of Health.https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/prediabetes-insulin-resistance#:~:text=Insulin%20resistance%20is%20when%20cells,help%20glucose%20enter%20your%20cells
Additional reporting by Amanda Chan, Live Science contributor
Follow Tia Ghose on Twitter and Google+. Follow LiveScience @livescience, Facebook & Google+.

Tia is the editor-in-chief (premium) and was formerly managing editor and senior writer for Live Science. Her work has appeared in Scientific American, Wired.com, Science News and other outlets. She holds a master's degree in bioengineering from the University of Washington, a graduate certificate in science writing from UC Santa Cruz and a bachelor's degree in mechanical engineering from the University of Texas at Austin. Tia was part of a team at the Milwaukee Journal Sentinel that published the Empty Cradles series on preterm births, which won multiple awards, including the 2012 Casey Medal for Meritorious Journalism.