Restrictions on fetal tissue research would threaten progress on breakthrough treatments for devastating diseases — and yet not prevent a single abortion
The U.S. government may restrict funding for research that uses human fetal tissue. The move would undermine medical science and prolong patients' suffering from devastating diseases.
Get the world’s most fascinating discoveries delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?

Delivered Daily
Daily Newsletter
Sign up for the latest discoveries, groundbreaking research and fascinating breakthroughs that impact you and the wider world direct to your inbox.

Once a week
Life's Little Mysteries
Feed your curiosity with an exclusive mystery every week, solved with science and delivered direct to your inbox before it's seen anywhere else.

Once a week
How It Works
Sign up to our free science & technology newsletter for your weekly fix of fascinating articles, quick quizzes, amazing images, and more

Delivered daily
Space.com Newsletter
Breaking space news, the latest updates on rocket launches, skywatching events and more!

Once a month
Watch This Space
Sign up to our monthly entertainment newsletter to keep up with all our coverage of the latest sci-fi and space movies, tv shows, games and books.

Once a week
Night Sky This Week
Discover this week's must-see night sky events, moon phases, and stunning astrophotos. Sign up for our skywatching newsletter and explore the universe with us!
Join the club
Get full access to premium articles, exclusive features and a growing list of member rewards.
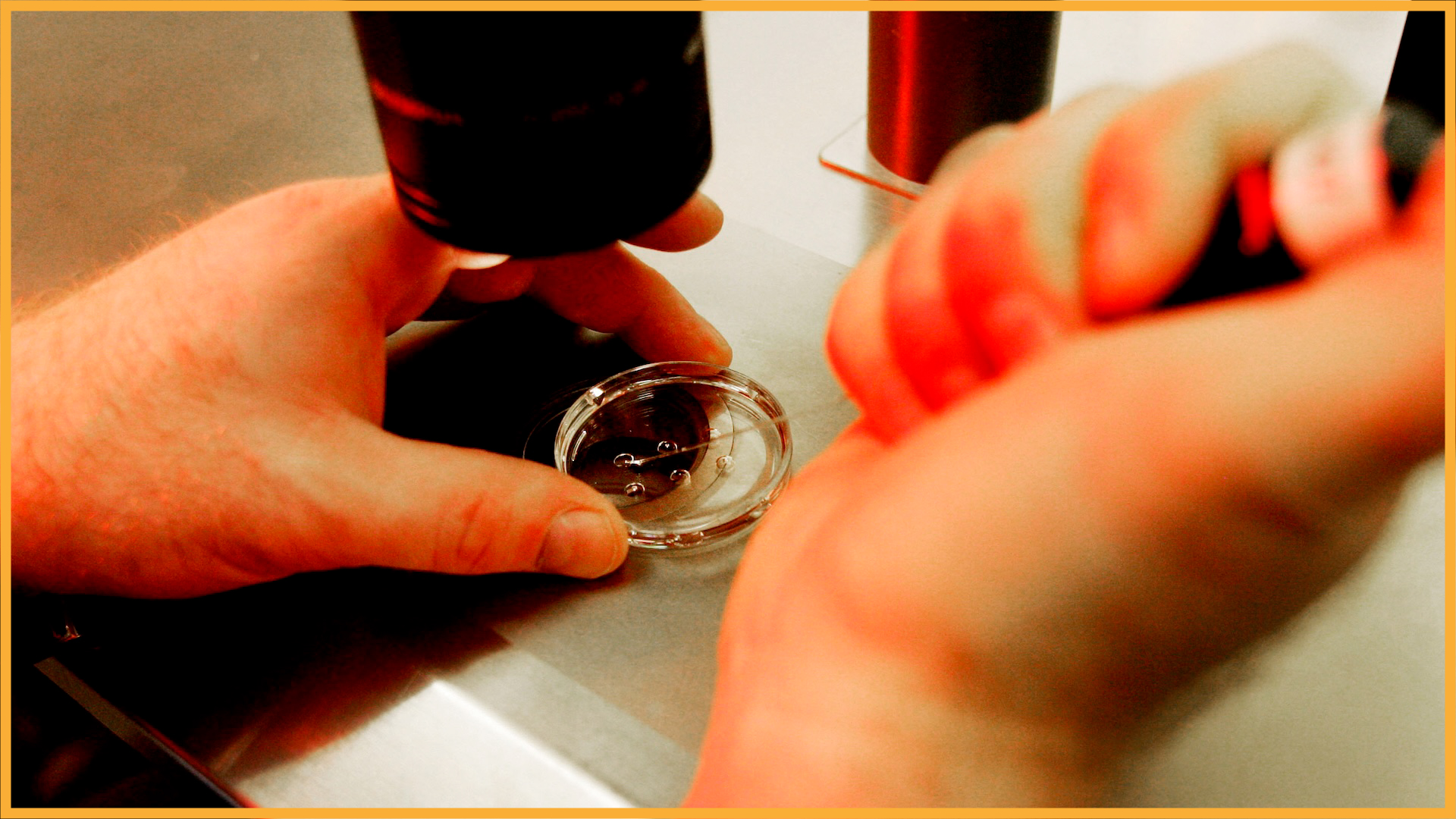
Human fetal tissue (HFT) research has been indispensable for understanding and combating diseases that affect millions worldwide. Reports that the National Institutes of Health (NIH) may not renew grants supporting this work are deeply troubling, as such action would jeopardize progress against devastating conditions including cancer, multiple sclerosis, Parkinson’s disease, eye disorders, and neurological and rare diseases.
For decades, HFT has been funded by the U.S. government. It’s had broad bipartisan support under both Republican and Democratic administrations because this research has saved lives. Yet, there are early signs that the Trump administration may ban ethical and well-established uses of fetal tissue in important medical research based on politics rather than science.
During Robert F. Kennedy Jr.’s Senate confirmation hearings, he committed to prohibiting research with HFT. And earlier this year, in its fiscal year 2026 budget proposal, the House Appropriations Labor-Health and Human Services Subcommittee included a policy rider that would restrict research with HFT. If successful, these efforts to ban fetal tissue research will serve only to prolong the suffering of people with terrible diseases.
HFT is irreplaceable. It allows scientists to study how human cells develop so they can recreate those processes using stem cells in the lab. Fetal cells are more resilient than adult cells and can be easier to grow making them essential for research. Most importantly, only human fetal cells accurately reveal how tissues and organs form because animal cells cannot replicate human development. For these reasons, HFT remains the gold standard for understanding human biology and disease.
There's an idea that restricting HFT research would somehow impact the prevalence of abortion in the U.S. — but restrictions on HFT research will not affect anyone’s decision about whether to terminate their pregnancy and will not prevent a single abortion. The research is conducted under strict ethical and scientific oversight. HFT may be obtained only after a woman has independently chosen to terminate a pregnancy, and tissue donation cannot be discussed until that decision is final.
Moreover, no financial incentives are permitted to encourage HFT donation. If not donated, the tissue is otherwise discarded. These restrictions ensure that research does not influence abortion decisions but allows ethically donated tissue to advance life-saving science.
The medical impact of HFT research is profound. In type 1 diabetes, which affects millions and costs $327 billion annually in the U.S., HFT has been crucial for understanding how insulin-producing pancreatic beta cells form and function. These insights have led to stem cell-derived beta cells now in clinical trials. HFT studies have also revealed how these cells respond to glucose (sugar) and why they may fail in people with diabetes — knowledge essential for developing durable therapies.
Get the world’s most fascinating discoveries delivered straight to your inbox.
HFT research has illuminated causes of and contributors to infertility and pregnancy complications such as preeclampsia, fetal growth restriction, and preterm birth — conditions that remain major public health challenges. Scientists have used HFT to develop stem cell-based models of placental development, which are impossible to replicate in animals. These models have revealed mechanisms that control placental formation and maternal-fetal interaction, paving the way for strategies to improve both maternal and child health.
Scientists cannot engineer effective therapies without first knowing how healthy tissues form. Animal models, though valuable, cannot fully mimic human organ development. Fetal tissue provides a window into that process and has enabled the creation of "humanized" models that incorporate authentic human cells to study the immune system, brain, skin and liver. These models, in turn, have advanced research into infectious diseases, cancer and regenerative medicine.
Neurodegenerative disease research has likewise advanced through HFT studies. Work using fetal tissue has identified early abnormalities that appear in fetuses' with Down syndrome and precede Alzheimer’s-like dementia, which routinely occurs in individuals with Down syndrome after age 40. These findings are informing strategies to prevent neurodegeneration before symptoms arise. In short, HFT uniquely bridges developmental and adult disease biology.
Perhaps the most striking examples of HFT’s value come from vaccine development. Nearly every major vaccine has relied at some stage on fetal-tissue-derived cells. Between 1960 and 2015, vaccines for polio, measles, mumps, rubella, varicella (chickenpox), herpes zoster (shingles), adenovirus, rabies, and hepatitis A prevented an estimated 4.5 billion cases of disease and 10.5 million deaths worldwide. The victory over polio — once a terrifying cause of paralysis and death — was possible only after scientists discovered that poliovirus replicated efficiently in fetal-tissue-derived cells. Likewise, the rubella vaccine, which prevents miscarriages and birth defects, was developed using an HFT-derived cell line that continues to ensure vaccine safety today.
HFT research has already saved millions of lives and continues to drive biomedical innovation. Restricting it would not alter abortion rates — it would only force scientists to discard an irreplaceable research resource instead of using it to advance treatments for devastating diseases. Science, not politics, should guide medical progress.
The choice is clear. We must continue to harness ethically donated human tissue to alleviate suffering and ensure that fear and misinformation do not stall life-saving discovery.
Lawrence S. B. Goldstein, PhD, is a cell biologist, geneticist, and neuroscientist renowned for pioneering work on molecular motors and transport pathways in neurodegenerative disease. After earning degrees from UC San Diego and the University of Washington, he held faculty positions at Harvard and UC San Diego. He co-founded the UCSD Stem Cell Program, Sanford Consortium for Regenerative Medicine, and Sanford Stem Cell Clinical Center. A longtime member of the International Society for Stem Cell Research (ISSCR), he is a member of the ISSCR Public Policy Committee, the namesake for the ISSCR Public Policy Fellowship program, has earned the American Society for Cell Biology Public Service Award, and is an elected member of the National Academy of Sciences.
You must confirm your public display name before commenting
Please logout and then login again, you will then be prompted to enter your display name.
 Live Science Plus
Live Science Plus





