Zika virus could potentially treat cancer, another early study hints
The Zika virus can target and eradicate human neuroblastoma tumors in a mouse model, a study shows. But how soon could such a treatment be used in people?
Get the world’s most fascinating discoveries delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?

Delivered Daily
Daily Newsletter
Sign up for the latest discoveries, groundbreaking research and fascinating breakthroughs that impact you and the wider world direct to your inbox.

Once a week
Life's Little Mysteries
Feed your curiosity with an exclusive mystery every week, solved with science and delivered direct to your inbox before it's seen anywhere else.

Once a week
How It Works
Sign up to our free science & technology newsletter for your weekly fix of fascinating articles, quick quizzes, amazing images, and more

Delivered daily
Space.com Newsletter
Breaking space news, the latest updates on rocket launches, skywatching events and more!

Once a month
Watch This Space
Sign up to our monthly entertainment newsletter to keep up with all our coverage of the latest sci-fi and space movies, tv shows, games and books.

Once a week
Night Sky This Week
Discover this week's must-see night sky events, moon phases, and stunning astrophotos. Sign up for our skywatching newsletter and explore the universe with us!
Join the club
Get full access to premium articles, exclusive features and a growing list of member rewards.
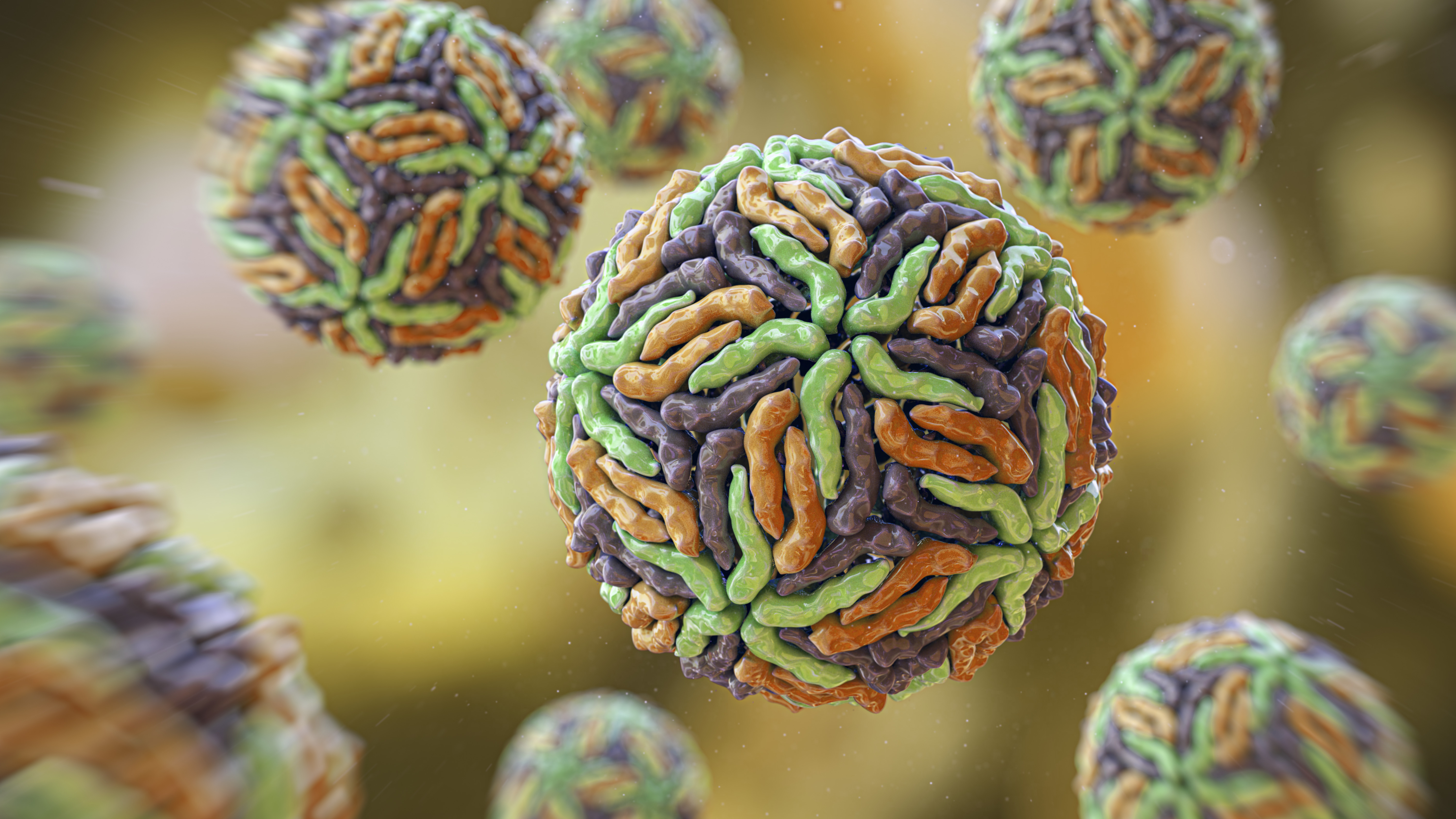
The Zika virus has plagued humans since its identification in 1947, but now, scientists are harnessing its ability to damage cells to fight a different foe: cancer.
In a new study published Jan. 9 in the journal Cancer Research Communications, researchers used the Zika virus to treat mice that had been implanted with cells from human neuroblastoma tumors, a type of nerve-tissue cancer. These mice's tumors showed almost complete tissue death immediately after they were injected with Zika, and the animals showed prolonged survival.
"The difference was stunning," Joseph Mazar, a research scientist at Nemours Children Hospital in Orlando, Florida, and first author of the study, told Live Science. "You just don't see this; it's crazy. We got 80% to 90% efficacy. The tumors were eradicated — single injection, no recurrence, no symptoms."
Researchers have investigated using Zika to kill cancer before — but how close is it to being a treatment used in human patients?
Related: Dormant cancer cells may 'reawaken' due to change in this key protein
Viruses as a cancer treatment
Using viruses as cancer treatment is not a new idea.
Since the 1800s, anecdotal reports have suggested that the health of some cancer patients improved following infection with certain viruses, such as influenza, hepatitis, measles or smallpox. Because of their ability to target and damage cancer cells, these viruses were dubbed oncolytic viruses, according to a 2023 review in the journal Biochimie.
Get the world’s most fascinating discoveries delivered straight to your inbox.
Early attempts to harness these viruses were unsuccessful, but in the 1990s, new genetic engineering techniques and lab-made DNA allowed researchers to tweak the viruses to be more specific and safer. Currently, only four viruses are approved as specific cancer treatments — for example, a modified herpes virus for malignant glioma is approved in Japan and another modified herpes virus for advanced melanoma is approved in the U.S. More cancer-killing viruses are in ongoing clinical trials.
So there's a precedent for treating cancer with viruses, but why use Zika?
The virus, which stunts brain growth in developing fetuses, targets immature nerve cells. This led Dr. Tamarah Westmoreland, a pediatric surgeon at Nemours Children Hospital and senior author of the study, and her team to determine whether they could use the virus to target neuroblastoma.
Neuroblastoma is a cancer that develops from immature nerve cells and is one of the most commonly diagnosed cancers in infants. Neuroblastoma development leads to poor survival rates despite intensive treatments. Most current treatments for high-risk tumors, which come with a poor prognosis, have severe side effects.
In the study, the researchers took high-risk neuroblastoma cells from human patients in which earlier treatments had failed and implanted them into mice that then developed tumors in their hind flanks. They then directly injected the tumors with an unmodified Zika virus. This consistently eradicated the tumors, without evidence of recurrence.
Most Zika infections are mild or cause no symptoms, and the mice did not experience any significant side effects following the treatment.
"What we see is, when we deliver it, the tumors are completely wiped out, and the surrounding tissue is totally normal," Mazar said.
"With very intensive therapies, [the children] have sustained so much to their body," Westmoreland told Live Science. "Zika virus can step in and serve as a bridge therapy at the time of radiation or surgery … and can clean up [what is left of] the high-risk neuroblastoma."
Neuroblastomas expressing high levels of a specific protein, called CD24, are especially vulnerable to cell damage and death by Zika infection, the study revealed. This protein is expressed by multiple cancers, opening possibilities for using the Zika virus against other tumor types.
"This work is exciting in that it suggests that the cell killing effects of Zika virus can be applied across cancer types, beyond what has previously been demonstrated," Dr. Milan Chheda, director of neuro-oncology at Washington University in St. Louis, told Live Science in an email. For now, though, "this adds a new tool to help patients with neuroblastoma, which is a devastating disease."
The treatment isn't ready for humans yet, but the researchers did try infecting human patients' extracted neuroblastoma tumors with Zika virus in the lab. According to Westmoreland and Mazar, the Zika virus did the same thing to the human tumors in the lab as it did in the mice.
"[Zika] is unique in that it is a perfect storm. What you have is something that has incredible specificity, but for specific types of cells, and if it's not that kind of cell, it does virtually nothing," Mazar said. "We have no reason to believe it wouldn't do this to a human tumor and a human person." While the researchers observed robust viral production within the tumor, there was very little viral shedding outside the tumor, implying that the Zika virus could be a safe alternative or add-on cancer therapy in people.
According to Westmoreland and Mazar, considering how effective the Zika virus was against human tumors in mice, we can hopefully expect to see the treatment in human trials in the next few years.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to community@livescience.com with the subject line "Health Desk Q," and you may see your question answered on the website!

Jennifer Zieba earned her PhD in human genetics at the University of California, Los Angeles. She is currently a project scientist in the orthopedic surgery department at UCLA where she works on identifying mutations and possible treatments for rare genetic musculoskeletal disorders. Jen enjoys teaching and communicating complex scientific concepts to a wide audience and is a freelance writer for multiple online publications.
 Live Science Plus
Live Science Plus










