What Is HPV?
Reference Article: Facts about HPV, or human papillomavirus.
Get the world’s most fascinating discoveries delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?

Delivered Daily
Daily Newsletter
Sign up for the latest discoveries, groundbreaking research and fascinating breakthroughs that impact you and the wider world direct to your inbox.

Once a week
Life's Little Mysteries
Feed your curiosity with an exclusive mystery every week, solved with science and delivered direct to your inbox before it's seen anywhere else.

Once a week
How It Works
Sign up to our free science & technology newsletter for your weekly fix of fascinating articles, quick quizzes, amazing images, and more

Delivered daily
Space.com Newsletter
Breaking space news, the latest updates on rocket launches, skywatching events and more!

Once a month
Watch This Space
Sign up to our monthly entertainment newsletter to keep up with all our coverage of the latest sci-fi and space movies, tv shows, games and books.

Once a week
Night Sky This Week
Discover this week's must-see night sky events, moon phases, and stunning astrophotos. Sign up for our skywatching newsletter and explore the universe with us!
Join the club
Get full access to premium articles, exclusive features and a growing list of member rewards.
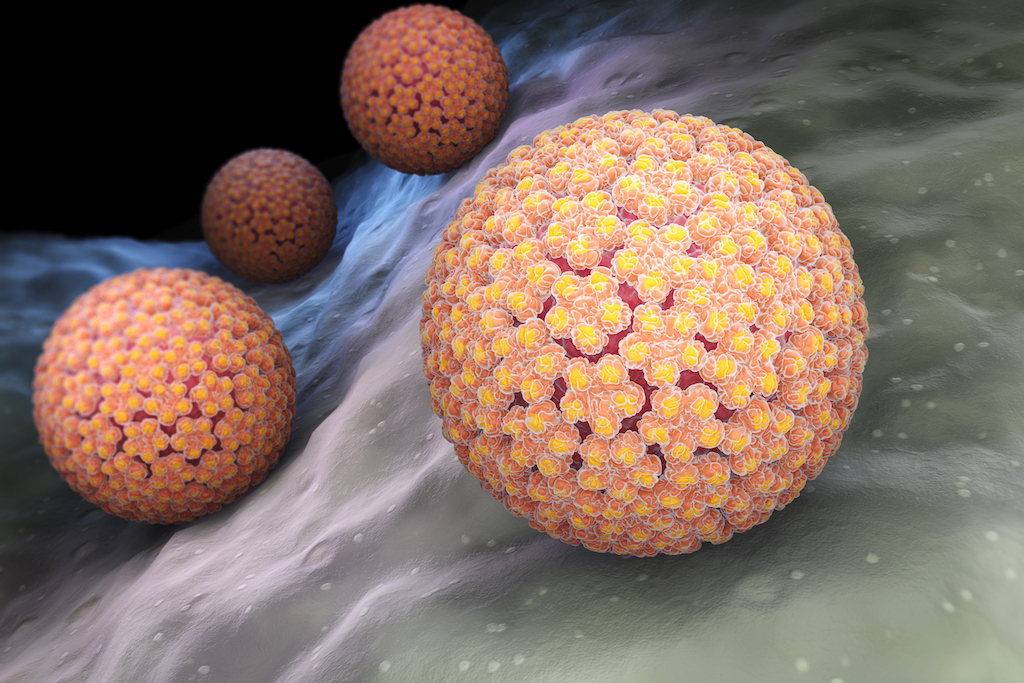
The human papillomavirus (HPV) is the most common sexually transmitted infection in the United States, according to the Centers for Disease Control and Prevention (CDC). Nearly 80 million people — about 1 in 4 adults in the U.S. — are currently infected with HPV, and 14 million people become newly infected each year in the U.S.
Most sexually active men and women will be infected with HPV at some point in their lives, and some may be infected repeatedly, according to the World Health Organization (WHO). A 2017 study published in the journal JAMA Oncology found that nearly half of American men under age 60 have an HPV infection.
There are more than 150 varieties of the human papillomavirus, and many types do not cause problems. Low-risk varieties usually clear up without any intervention, and 90% of infections clear up within two years without treatment. However, at least 14 types of HPV are high risk, according to the WHO, and these infections can persist and lead to cancer. Researchers from the CDC discovered that 23% of the participants in a 2017 health survey were infected with a high risk strain of genital HPV.
How HPV is transmitted
HPV is contracted through skin-to-skin contact, most commonly sexual contact, such as vaginal, anal or oral sex. People of all genders and sexual orientations can become infected with HPV.
"Both men and women can acquire the infection, and since HPV is the most common sexually transmitted infection in the U.S. and in the world, almost all females and males will be infected with at least one type of HPV at some point in their lives," Dr. Barbara Pahud, associate director of the vaccine unit at Children's Mercy Hospital in Kansas City, Missouri, told Live Science.
HPV warts
Though most people with HPV don't have symptoms, some develop warts, or papillomas. This symptom varies depending on the type of virus and can include genital warts, common warts and plantar warts (hard, grainy growths on the feet).
Of the more than 150 strains of HPV, 40 affect the genitals, according to NYU Langone Health. HPV 6 and HPV 11 are the types of HPV that cause 90% of all genital warts.
Get the world’s most fascinating discoveries delivered straight to your inbox.
Regardless of whether there are obvious symptoms, the virus may lead to other, more serious health conditions, such as cervical, vaginal and vulvar cancers in women and penile cancer in men. Anal cancer, cancer of the back of the throat (oropharynx) and genital warts can also be caused by HPV in both men and women.
The virus is the only known cause of cervical cancer in women. HPV types 16 and 18 cause 70% of precancerous cervical lesions and cervical cancers, according to the WHO.
HPV "typically invades a specific area of the cervix referred to as the transitional zone," said Dr. Eric M. Genden, a professor and chairman of otolaryngology head and neck surgery at the Icahn School of Medicine at Mount Sinai in New York. "This is an area of high cellular turnover. While the virus integrates into the patient's DNA, the virus typically runs a course of brief infection and then passes. In select few, the virus may persist and result in chronic infection. In those who develop a chronic infection, carcinoma [cancer] may develop."
Typically, women develop a robust immune response to the HPV infection, and fewer women develop viral-related infections compared to men, Genden said. Men, in contrast, do not always exert a strong immune response to the infection.
Diagnosis
In women, HPV can be diagnosed after a Pap smear, Dr. Sherry Ross, an OB-GYN and women's health expert in Santa Monica, California, told Live Science.
HPV is found more often in women than in men because cervical screening is part of a regular gynecological exam, Ross said. Men don't have regular pelvic or genital examinations, making HPV less likely to be found. However, "anal Pap smear testing can be done for those men who are high-risk or have anal sex," Ross said.
How to prevent HPV
Using protection such as condoms and dental dams (latex sheets used during oral sex) can lower the risk of HPV transmission during sex. These methods can be used during any skin-to-skin sexual contact, but they aren't foolproof.
The best way to prevent HPV is with the vaccine. The CDC recommends that boys and girls receive the HPV vaccine at age 11 or 12 so they are protected before potentially being exposed to the virus. Plus, when the vaccine is given to preteens, it produces a more robust immune response than it does in older people.
Until 2018, the HPV vaccine was recommended through age 26 for women, through age 21 for heterosexual men, and through age 26 for people with compromised immune systems and for men who have sex with men.
Recently, however, the Food and Drug Administration (FDA) approved the vaccine for adults up to age 45 based on a study of approximately 3,200 women (ages 27 to 45) who were followed for an average of 3.5 years. The study found that the vaccine Gardasil was 88% effective in the prevention of persistent infection, genital warts, vulvar and vaginal precancerous lesions, cervical precancerous lesions, and cervical cancer related to HPV types covered by the vaccine.
U.S. doctors are strongly in favor of the use of the HPV vaccine as a method of cervical cancer prevention. A poll of 1,952 U.S. doctors by SERMO, a social media network for doctors, found that 55% of doctors favored state mandates for HPV vaccination. In addition, 92% of doctors confirmed that they would vaccinate their own children, despite controversy over the safety of the HPV vaccine. The HPV-9 vaccine can prevent around 80% of the viruses that cause cervical cancer.
A 2017 case report published in the journal JAMA Dermatology suggested that the HPV vaccine may even help to prevent skin cancer. However, the report described the cases of only two patients, so much larger studies are needed to confirm the findings.
Side effects of the vaccine, when they do occur, are typically very mild. They include pain, redness or swelling in the arm where the shot was given, fever, headache, fatigue and muscle or joint pain, Genden said.
"With all vaccines, it hurts to get a shot in the arm, but that passes," Pahud said. "Teens also may faint after vaccination, but not due to the HPV vaccine itself but the injection procedure. These findings are similar to the safety reviews of the other two recommended teen vaccines: meningococcal vaccines and tetanus booster vaccines."
Additional resources:
- Watch "HPV Vaccine: Ask About it For Your Child," from the CDC.
- Read more about HPV and cancer from the National Cancer Institute.
- Learn more about sexually transmitted diseases and how to prevent them, from the CDC.
This article was updated on Aug. 27, 2019 by Live Science Contributor Traci Pedersen. This article is for informational purposes only and is not meant to offer medical advice.

 Live Science Plus
Live Science Plus