Gay Men Who Use Hook-Up Apps Have Higher STD Risk
Get the world’s most fascinating discoveries delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?

Delivered Daily
Daily Newsletter
Sign up for the latest discoveries, groundbreaking research and fascinating breakthroughs that impact you and the wider world direct to your inbox.

Once a week
Life's Little Mysteries
Feed your curiosity with an exclusive mystery every week, solved with science and delivered direct to your inbox before it's seen anywhere else.

Once a week
How It Works
Sign up to our free science & technology newsletter for your weekly fix of fascinating articles, quick quizzes, amazing images, and more

Delivered daily
Space.com Newsletter
Breaking space news, the latest updates on rocket launches, skywatching events and more!

Once a month
Watch This Space
Sign up to our monthly entertainment newsletter to keep up with all our coverage of the latest sci-fi and space movies, tv shows, games and books.

Once a week
Night Sky This Week
Discover this week's must-see night sky events, moon phases, and stunning astrophotos. Sign up for our skywatching newsletter and explore the universe with us!
Join the club
Get full access to premium articles, exclusive features and a growing list of member rewards.
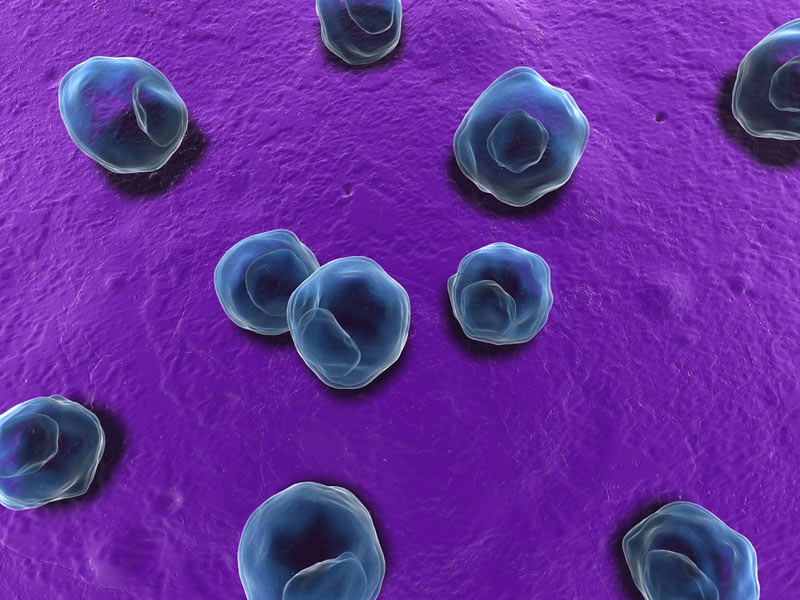
Gay men who hook up by using smartphone apps may be at higher risk for some sexually transmitted infections than men who find sexual partners through online dating, or in bars and clubs, a new study suggests.
In the study, which involved gay and bisexual men, those who used smartphone apps (such as Grindr and Recon) to find sexual partners were 23 percent more likely to be infected with gonorrhea, and 35 percent more likely to be infected with chlamydia, compared with men who met sexual partners in bars, clubs and other in-person venues.
Men who used smartphone apps for hook ups were also about 40 percent more likely to be infected with gonorrhea compared with those who used Internet websites (such as Manhunt and Adam4Adam) to meet sexual partners. [Sexy Tech: 6 Apps That May Stimulate Your Love Life]
The smartphone apps — which use a phone's GPS to locate nearby users — may allow people to meet sexual partners more quickly and easily than other methods, and so increase the chances of hooking up with strangers and acquiring sexually transmitted diseases, the researchers said.
"Technological advances which improve the efficiency of meeting anonymous sexual partners may have the unintended effect of creating networks of individuals where users may be more likely to have sexually transmissible infections," the researchers, from the L.A. Gay & Lesbian Center in Los Angeles, wrote in a paper published online today (June 12) in the journal Sexually Transmitted Infections.
But public health workers may be able to use the same technologies to encourage STD testing, the researchers said. There is already an app called Hula that allows users to find STD testing centers and share their results with potential sex partners.
"Technology is redefining sex on demand — prevention programs must learn how to effectively exploit the same technology," the researchers said.
Get the world’s most fascinating discoveries delivered straight to your inbox.
Previous studies have found that gay and bisexual men who use the Internet to meet sex partners are more likely to engage in unprotected sex and have a higher number of sex partners than those who meet sex partners in more traditional ways.
The new study involved more than 7,100 gay and bisexual men who were tested for STDs at a sexual health center in Los Angeles between 2011 and 2013, and who answered questions about their use of social networking to meet sexual partners.
About one-third of the participants, 34 percent, met sex partners only in real life (at bars, clubs, etc.); 30 percent met sex partners both in real life and through Internet websites; and 36 percent met sex partners through smartphone apps as well as other methods.
There was no link between smartphone app use and the risk of some other STDs, such as HIV and syphilis, according to the study.
Because the study involved men who visited a sexual health clinic, and who lived in a big city, the results may not necessarily apply to other populations, such as those in rural areas, the researchers said.
Follow Rachael Rettner @RachaelRettner. Follow Live Science @livescience, Facebook & Google+. Original article on Live Science.

Rachael is a Live Science contributor, and was a former channel editor and senior writer for Live Science between 2010 and 2022. She has a master's degree in journalism from New York University's Science, Health and Environmental Reporting Program. She also holds a B.S. in molecular biology and an M.S. in biology from the University of California, San Diego. Her work has appeared in Scienceline, The Washington Post and Scientific American.
 Live Science Plus
Live Science Plus