New 'Nightmare' Bacteria Are Popping Up All Over the US
Get the world’s most fascinating discoveries delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?

Delivered Daily
Daily Newsletter
Sign up for the latest discoveries, groundbreaking research and fascinating breakthroughs that impact you and the wider world direct to your inbox.

Once a week
Life's Little Mysteries
Feed your curiosity with an exclusive mystery every week, solved with science and delivered direct to your inbox before it's seen anywhere else.

Once a week
How It Works
Sign up to our free science & technology newsletter for your weekly fix of fascinating articles, quick quizzes, amazing images, and more

Delivered daily
Space.com Newsletter
Breaking space news, the latest updates on rocket launches, skywatching events and more!

Once a month
Watch This Space
Sign up to our monthly entertainment newsletter to keep up with all our coverage of the latest sci-fi and space movies, tv shows, games and books.

Once a week
Night Sky This Week
Discover this week's must-see night sky events, moon phases, and stunning astrophotos. Sign up for our skywatching newsletter and explore the universe with us!
Join the club
Get full access to premium articles, exclusive features and a growing list of member rewards.
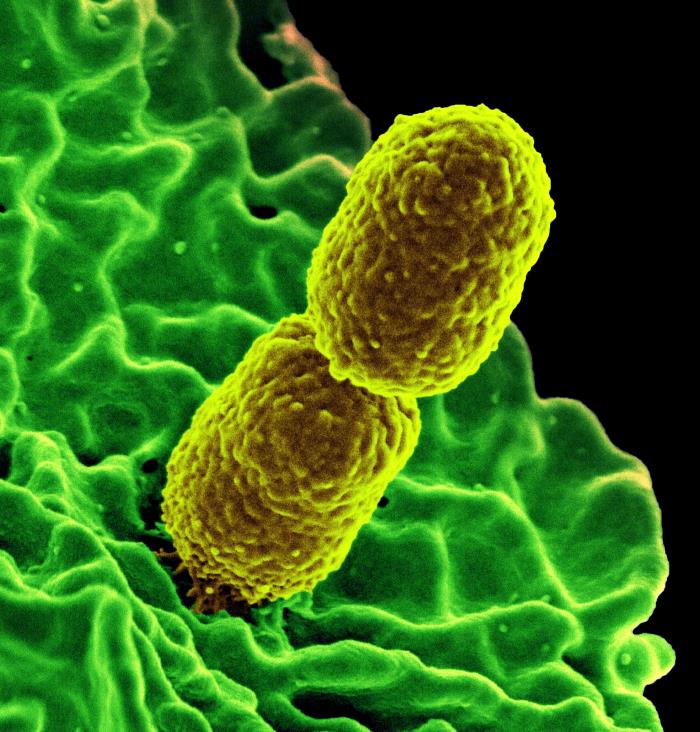
What's worse than "nightmare" bacteria that are resistant to nearly all antibiotics? New nightmare bacteria that have the potential to spread their resistance genes to germs in hospitals around the country.
Researchers say that last year, they identified more than 200 cases of these "nightmare" bacteria with new or rare antibiotic-resistance genes, according to a new report from the Centers for Disease Control and Prevention (CDC). These rare types of antibiotic-resistant bacteria popped up all over the country, in 27 states.
The good news is that researchers have come up with an aggressive strategy to identify, track and contain these germs, which appears to help stop their spread, according to the report.
"We are working to get in front of them before they do become common," Dr. Anne Schuchat, principal deputy director of the CDC, said at a news conference today (April 3). "We have data showing an aggressive approach works" to halt the spread of these new threats, Schuchat said. [6 Superbugs to Watch Out For]
Nightmare bacteria
Antibiotic-resistant bacteria are, unfortunately, a common problem in medicine today — more than 2 million Americans get an antibiotic-resistant infection each year, and 23,000 die from these infections, according to the CDC. Antibiotic-resistant infections are a major concern for health care workers because they are difficult to treat.
One particularly concerning type of antibiotic-resistant bacteria is called carbapenem-resistant Enterobacteriaceae, or CRE, which has been dubbed "nightmare" bacteria. These bacteria are not only resistant to many antibiotics but are also highly lethal, killing up to 50 percent of infected patients, according to the CDC.
Doctors liken the spread of CRE and other antibiotic-resistant germs to a wildfire, which is difficult to contain once it spreads widely. Therefore, doctors are trying to stamp out new or unusual types of antibiotic resistance when they first appear — to extinguish the "spark" before it has a chance to grow and spread, Schuchat said.
Get the world’s most fascinating discoveries delivered straight to your inbox.
To aid in these efforts, the CDC recently established the Antibiotic Resistance Laboratory Network (ARLN), a network of labs across the country that test patients' samples for highly resistant bacteria and track emerging antibiotic resistance.
In the first nine months of 2017, ARLN tested more than 5,700 samples of highly resistant bacteria, including CRE, from hospitals, nursing homes and other health care facilities around the country. Of the 1,400 CRE-positive samples tested, 221 samples (15 percent) had new or unusual types of antibiotic resistance, the report said.
"I was surprised by the numbers" of bacteria with unusual antibiotic resistance, Schuchat said. "This was more than I was expecting."
When researchers detected a case of unusual antibiotic resistance, they screened other patients in the facility to see if some had "silent" infections, meaning they were infected but weren't showing symptoms. They found that about 1 in 10 people screened had a silent infection, meaning that "unusual resistance may have spread and could have continued spreading if left undetected," Schuchat said.
Preventing spread
Fortunately, researchers were often able to stop the spread of these unusual antibiotic-resistant bacteria with an aggressive "containment" strategy. This strategy involves rapidly identifying antibiotic-resistant germs at a given facility, assessing the facility for gaps in infection control, screening other patients to see if any are "silent" carriers of the infection, coordinating a response with other facilities in the area that may transfer patients to and from the affected facility, and continuing these steps until transmission of the antibiotic-resistant bacteria is controlled.
This containment strategy can "help stop the spread of unusual types of antibiotic resistance that haven't yet spread widely," Schuchat said.
Using a mathematical model, the researchers estimated that implementing this strategy could prevent as many as 1,600 new CRE infections in three years, or a 76-percent reduction in cases.
Schuchat stressed that efforts to fight antibiotic resistance are ongoing.
"We need to do more, and we need to do it faster and earlier with each new antibiotic-resistance threat," Schuchat said.
Original article on Live Science.

Rachael is a Live Science contributor, and was a former channel editor and senior writer for Live Science between 2010 and 2022. She has a master's degree in journalism from New York University's Science, Health and Environmental Reporting Program. She also holds a B.S. in molecular biology and an M.S. in biology from the University of California, San Diego. Her work has appeared in Scienceline, The Washington Post and Scientific American.
 Live Science Plus
Live Science Plus