6 Superbugs to Watch Out For
Introduction
Superbugs, also known as drug-resistant bacterial infections, can cause infections that are hard to treat. These clever germs have found ways to survive in the face of treatments with antibiotics, the drugs that usually kill bacteria.
In fact, according to the Centers for Disease Control and Prevention (CDC), all bacterial infections in the world are slowly becoming resistant to antibiotic treatments. That's because disease-causing bacteria are living organisms that constantly evolve, enabling them to adapt to new environments. Antibiotic resistance develops over time — it can start from even a very small number of microbes within a population that have genes that allow them to continue to grow, despite the use of drugs that would normally kill them.
Researchers suggest that some microbes are able to survive antibiotic treatments because they swap genes with each other, making them drug-resistant.
In any case, the bacteria that survive an antibiotic treatment eventually outnumber the population of bacteria that are susceptible to the drug.
Here are 6 superbugs that can be challenging to treat.
Klebsiella pneumoniae

Klebsiella pneumoniaebacteria can infect the lungs and lead to pneumonia. The bacteria can also infect wounds or surgical sites, or spread through the body via blood infections.
Normally, Klebsiella bacteria can be found in humans'[s1] mouths, intestines and skin, and they cause no harm to people with healthy immune systems. But certain strains, like Klebsiella pneumoniae, can be dangerous for some people with weakened immune systems, particularly those in hospitals.
Get the world’s most fascinating discoveries delivered straight to your inbox.
One strain of the bacteria is also resistant to a number of antibiotics, making the infection hard to treat. This type of Klebsiella pneumoniae produces an enzyme known as carbapenemase, which prevents antibiotics called carbapenems from killing the bacteria and treating the infection.
To prevent spread of infection, the CDC recommends patients and hospital personnel follow strict hygiene procedures, such as hand-washing and wearing hospital gowns and gloves.
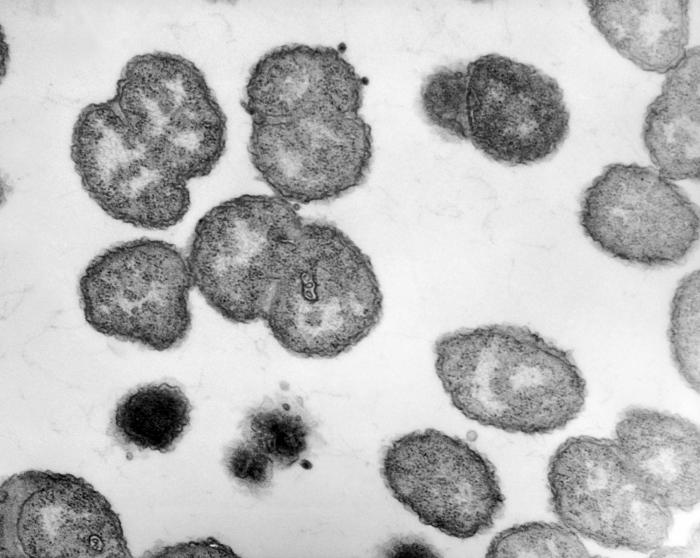
Methicillin-resistant Staphylococcus aureus

MRSA, which stands for methicillin-resistant Staphylococcus aureus, is a strain of bacteria that's resistant to the antibiotics used to treat typical staph infections. The bacteria can spread by touching, as often occurs in hospitals.
Once the bacteria enters the body, they can spread to bones, joints or major organs such as the lungs, heart or brain.
The rate of MRSA infections in hospital patients has increased in recent years, according to a recent study published in the August issue of the journal Infection Control and Hospital Epidemiology. Results showed that in 2003, an average of 21 out of every 1,000 hospital patients developed an infection. The number jumped up to 42 out of 1,000 patients in 2008.
The best way to prevent the spread of MRSA is for health care workers and hospital visitors to keep their hands clean, according to the CDC.
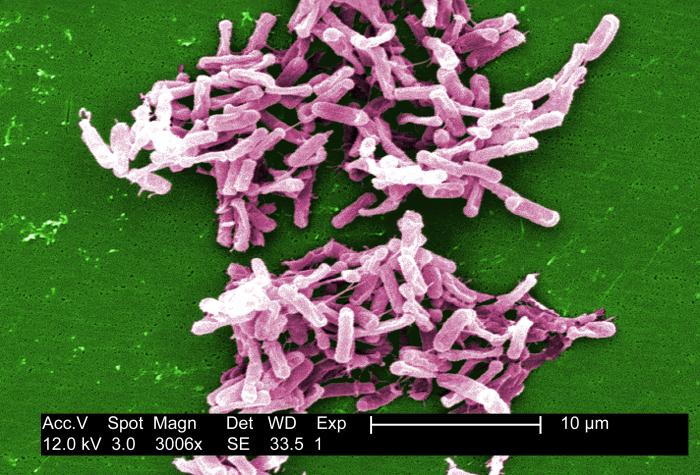
Clostridium difficile
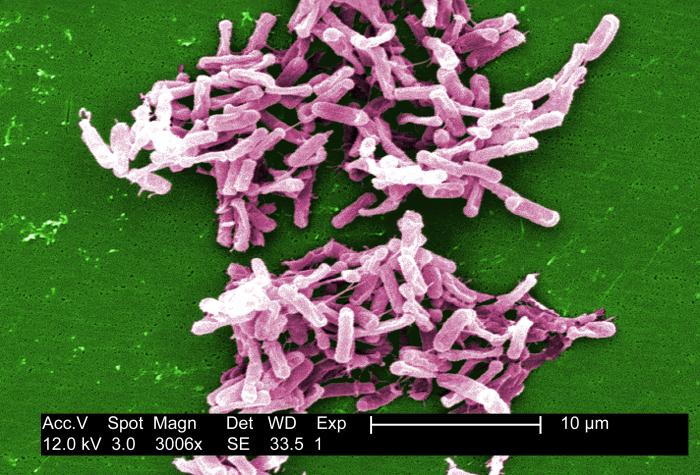
Clostridium difficilebacteriaare found in the intestines. Healthy people who have enough "good" bacteria in their intestines may not get sick from a C. diff infection. But for people with weak immune systems, the germ can cause a number of symptoms, such as diarrhea or life-threatening inflammation of the colon.
People who take antibiotics are at greater risk of C. diff infection, because antibiotics can kill the good germs in the intestines, leaving an imbalance.
C. difficilecan cause severe diarrhea, and the germ is linked to 14,000 American deaths each year, according to the CDC.
Those most at risk are the elderly who take antibiotics, and also those who get regular hospital care.[s2]
In about one in four patients, the infection may go away within two to three days after stopping antibiotic use, according to the CDC. Once the infection is gone, doctors generally prescribe another antibiotic for 10 days to make sure the infection doesn't return.
Extensively Drug Resistant Tuberculosis
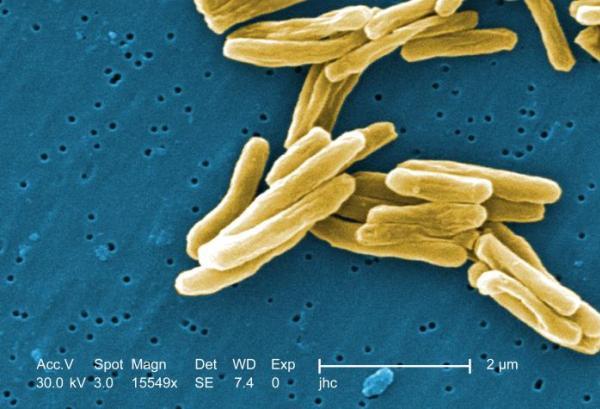
Extensively drug-resistant tuberculosis (XDR TB) is rare type of tuberculosis that is resistant to a number of antibiotic drugs. This resistance leaves fewer treatment options available, which can increase the risk of death.
Tuberculosis is a contagious bacterial infection that involves the lungs, but can spread to other organs. A person with TB releases the bacteria into the air when they cough or sneeze, and the germs can float for several hours. People who breathe in the air containing the bacteria can become infected.
A total of 10,528 TB cases were reported in the U.S. in 2011, according to the CDC.
People who don’t take their TB medications regularly [s3] are at greater risk of getting drug-resistant TB.
Drug-resistant Gonorrhea
Gonorrhea is a sexually transmitted disease that is caused by the bacteria Neisseria gonorrhoeae.
Over time, gonorrhea bacteria have developed a resistance to antibiotics such as sulfonilamides, penicillin, tetracycline and ciprofloxacin, which are commonly prescribed to treat gonorrhea infections.
Recently, the CDC stopped recommending the use of an antibiotic called cefixime to treat gonorrhea, because the drug was losing its effectiveness. Now, they recommend treating infections with a drug called ceftriaxone, along with either azithromycin or doxycycline, as the best way to reduce the risk of the bacteria becoming even more drug-resistant.
In 2010, a total of 309,341 cases of gonorrhea were reported in the U.S. — a rate of about one case per 1,000 people, according to the CDC.
Shiga toxin-producing Escherichia coli
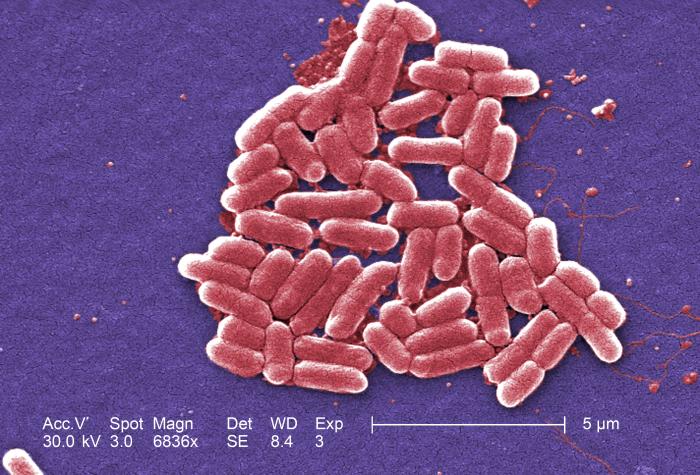
Escherichia coli are a large group of bacteria, and some normally live in the intestines of people and animals.
Although some strains of the bacteria are harmless, others can make you sick. They can cause diarrhea, urinary tract infections, respiratory illness and pneumonia.
One harmful strain is the Shiga toxin-producing E. coli, also known as STEC, which live in the guts of animals such as cattle, goats, sheep, deer and elk. Humans can become infected by eating contaminated food, drinking raw milk or contaminated water, coming in contact with cattle or with the feces of infected people.
STEC are resistant to a number of classes of antibiotics. In fact, antibiotic treatment is generally discouraged because it may increase the risk of developing hemolytic uremic syndrome, a disorder that can destroy red blood cells, causing damage to the kidneys.
An estimated 265,000 STEC infections occur yearly in the U.S., reports the CDC.
Earlier this year, an outbreak of a particular strain of STEC, called E. coli O145, was identified in nine states. A total of 18 people were infected, four were hospitalized and one person in Louisiana died.
To prevent STEC infections, the CDC recommends washing hands thoroughly after using the bathroom or preparing food, cooking meats thoroughly and avoiding drinking raw milk.
Follow MyHealthNewsDaily on Twitter @MyHealth_MHND. Find us on Facebook.
 Live Science Plus
Live Science Plus





