Frozen Poop Is As Good As Fresh Poop for C. Difficile Treatment
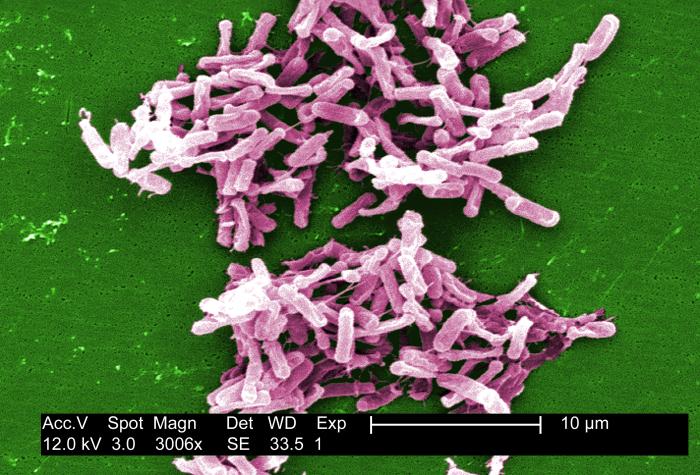
For patients with the difficult-to-treat intestinal infection caused by a bacterium called Clostridium difficile, a "poop transplant" that uses frozen poop may be as effective as one that uses fresh poop, a new study suggests.
Frozen-poop transplants have a number of advantages over fresh-poop transplants for use in patients with C. difficile, said study author Dr. Christine Lee, an infectious-disease specialist at McMaster University in Ontario, Canada.
In the study, researchers looked at more than 200 adults who had C. difficile infections that were recurrent or unresponsive to other types of treatment. The researchers found that the percentage of patients who recovered from their infection without relapsing about three months after receiving frozen fecal transplants from healthy donors was comparable to the percentage of those who recovered after receiving fresh fecal transplants. [5 Things Your Poop Says About Your Health]
The people who donate the fecal material that is used for such transplants have to undergo extensive medical testing, including blood and stool testing, and that can take one to two weeks, Lee told Live Science. But if the material can be frozen and stored, it can be available for use right away when a patient needs it, even in facilities that don't have the labs needed to prepare fecal material for transplants, she said.
Infections with C. difficile are notoriously difficult to treat, and patients have high rates of recurrences even if their symptoms initially improve. The bacterium is one of the most common causes of infection of the colon, and more than 60 percent of patients who have been infected with it experience further episodes, researchers estimate.
In the new study, 114 adults with recurrent or treatment-resistant C. difficile infections received frozen-poop transplants, and 118 adults received fresh-poop transplants, via enemas. Some in each group also received antibiotics.
Among the patients who received frozen transplants and antibiotics, 75 percent experienced a resolution of the main symptom of their infection (diarrhea) after 13 weeks, compared with 70 percent of those who received fresh-poop transplants and antibiotics.
Get the world’s most fascinating discoveries delivered straight to your inbox.
Among the patients who did not receive antibiotics, 83.5 percent of the patients who received frozen transplants experienced a resolution of their diarrhea after 13 weeks, compared with 85 percent of those who received fresh-poop transplants.
Previous research has suggested that frozen-poop transplants could be as effective as fresh ones, but that research was conducted in a much smaller number of participants than in the new study, Lee said. Therefore, the data from the new study "is more robust," she told Live Science.
Now, the researchers are planning to test the effectiveness of transplants involving poop that has been frozen and dried, Lee said. One advantage of this technique would be a longer shelf life and the possibility of sending the material to any location in the world, she said.
The new study was published today (Jan. 12) in the journal JAMA.
Follow Agata Blaszczak-Boxe on Twitter. Follow Live Science @livescience, Facebook & Google+. Originally published on Live Science.


