Teen's year-long case of depression and seizures caused by brain-injuring autoimmune disease
After she'd spent a year experiencing unusual mood and behavioral symptoms, doctors discovered the teen's brain was being attacked by her own cells.
Get the world’s most fascinating discoveries delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?

Delivered Daily
Daily Newsletter
Sign up for the latest discoveries, groundbreaking research and fascinating breakthroughs that impact you and the wider world direct to your inbox.

Once a week
Life's Little Mysteries
Feed your curiosity with an exclusive mystery every week, solved with science and delivered direct to your inbox before it's seen anywhere else.

Once a week
How It Works
Sign up to our free science & technology newsletter for your weekly fix of fascinating articles, quick quizzes, amazing images, and more

Delivered daily
Space.com Newsletter
Breaking space news, the latest updates on rocket launches, skywatching events and more!

Once a month
Watch This Space
Sign up to our monthly entertainment newsletter to keep up with all our coverage of the latest sci-fi and space movies, tv shows, games and books.

Once a week
Night Sky This Week
Discover this week's must-see night sky events, moon phases, and stunning astrophotos. Sign up for our skywatching newsletter and explore the universe with us!
Join the club
Get full access to premium articles, exclusive features and a growing list of member rewards.
A teenage girl suddenly began experiencing depression, seizures and involuntary episodes in which she'd hit her head or scratch her arms and then not recall doing so. Doctors discovered that her symptoms actually stemmed from brain inflammation caused by a common autoimmune disease, a new case report reveals.
The 15-year-old girl, from Taiwan, was hospitalized after experiencing a year-long decline in mood, repeated seizures and sudden bursts of these involuntary, self-injuring behaviors, up to three times a day. After many tests, her doctors concluded she had Sjögren's syndrome (SS), an autoimmune disease that most commonly affects the tear and salivary glands but can also impact the central nervous system (CNS), which includes the brain and spinal cord.
According to the case report, published June 29 in the journal Frontiers in Immunology, finally getting an accurate diagnosis and appropriate treatment meant the teen was able to recover and get her life "back on track," as she reportedly phrased it to her doctors.
Related: Woman who spontaneously vomited up to 30 times a day likely had rogue antibodies
SS occurs when the body's immune system attacks fluid-producing glands, like those that make tears and saliva, leading to symptoms of dry mouth and eyes, fatigue and joint pain, according to the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Estimated to affect up to 3% of adults worldwide, the disease is usually diagnosed in people age 40 or older, and it affects mainly women. SS can sometimes lead to neuropsychiatric symptoms in adults by damaging the CNS. However, similar complications have rarely been studied in young people.
In the new case, the girl had a history of epilepsy related to a past bacterial infection that had been successfully treated. One year prior to being diagnosed with SS, the teen noticed her confidence had dropped, her mood worsened, and she struggled to sleep and remember things.
After experiencing three seizures, doctors prescribed her antiepileptic medication that initially improved her symptoms, but the effects didn't last. She started to have "episodes" where she would suddenly become agitated and start unconsciously harming herself. Sometimes, just before her mood or behavior changed, the patient experienced a sudden shift in perception, called an "aura," which in her case involved flashes of light or machine sounds. Scans showed that these mood and behavior shifts were linked to bursts of seizure-inducing electrical activity in the brain.
Get the world’s most fascinating discoveries delivered straight to your inbox.
However, despite this harmful electrical activity, further brain scans found no evidence of structural damage on her brain, and there were no abnormalities in her cerebrospinal fluid (CSF), the clear fluid that cushions the brain and spinal cord. Doctors also ruled out viral infection, thyroid issues and cancer as potential causes. Believing that the patient was likely experiencing brain inflammation, the team prescribed anti-inflammatory drugs, which partially improved her mood, but her agitation and self-injuring episodes returned.
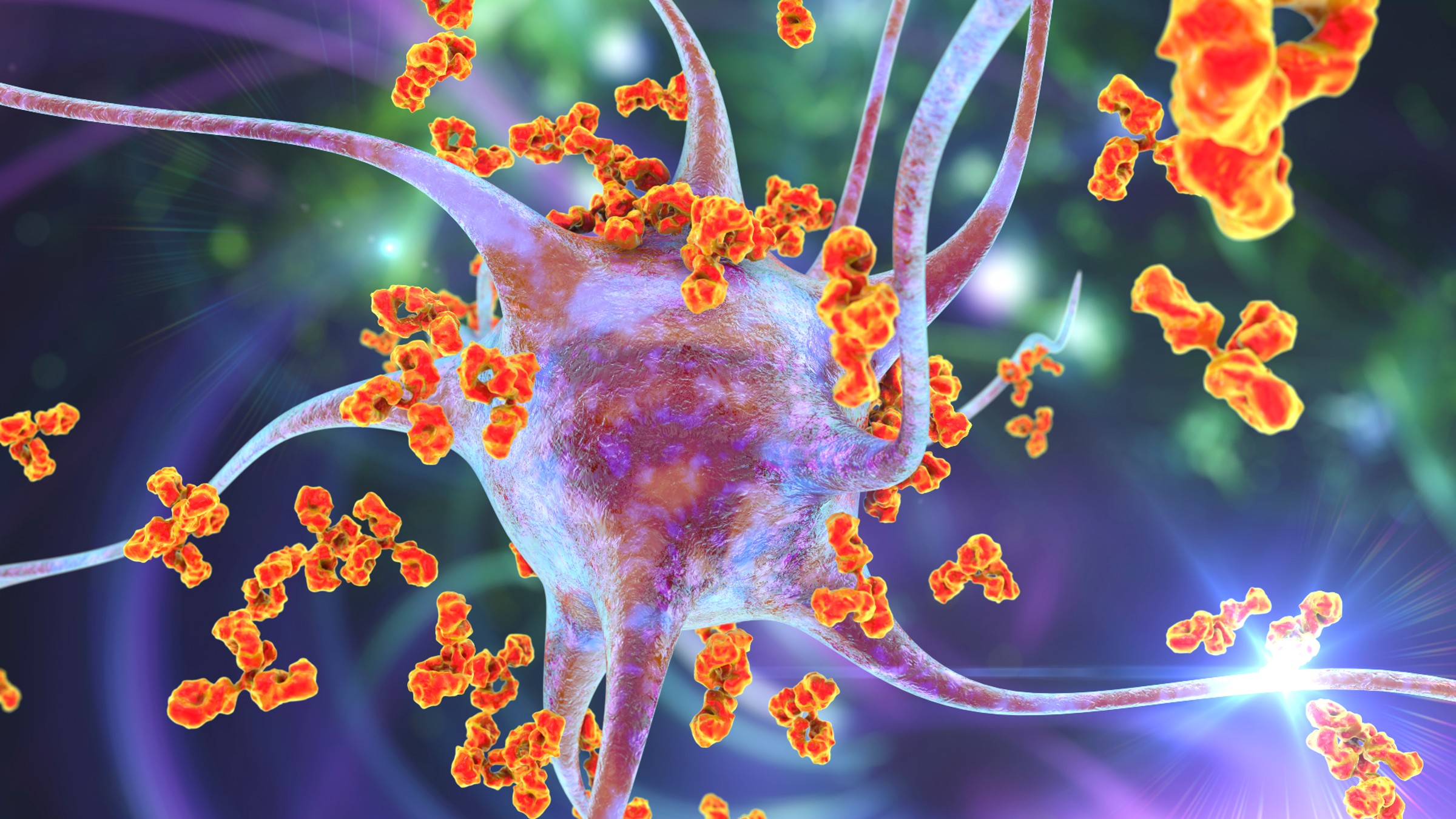
At this point, the doctors screened the patient's blood and CSF again and discovered specific autoantibodies — antibodies that attack the body rather than foreign invaders. The patient also had a dry mouth and eyes, leading the team to conclude that she had SS. More specifically, SS was causing a type of brain inflammation resulting from an immune attack on the organ's cells, known as autoimmune encephalitis. After starting an immune-suppressing therapy, the girl's mood improved and her self-injuring episodes stopped.
Although SS is most prevalent in adults, the team hopes that the case will raise awareness of the condition in teenagers.
"We emphasize the critical importance of physicians remaining vigilant regarding the possibility of underlying physical conditions when encountering sudden instances of self-harm behavior that appear to be out of context," senior author Dr. Chun-Hao Liu, a psychiatrist from the Chang Gung Memorial Hospital at Linkou, told Live Science in an email. "It is imperative to consider various encephalopathies [brain damage or disease], alongside psychiatric disorders, as potential underlying factors in individuals displaying abrupt behavioral changes, as overlooking these medical conditions could lead to misdiagnoses."

Emily is a health news writer based in London, United Kingdom. She holds a bachelor's degree in biology from Durham University and a master's degree in clinical and therapeutic neuroscience from Oxford University. She has worked in science communication, medical writing and as a local news reporter while undertaking NCTJ journalism training with News Associates. In 2018, she was named one of MHP Communications' 30 journalists to watch under 30.
 Live Science Plus
Live Science Plus










