New RSV shots tied to rare nervous system disorder — should you worry?
There's been some reports of Guillain-Barré syndrome in older adults who got the vaccines. But health officials still recommend that this population get the shots, in consultation with their doctors.

Get the world’s most fascinating discoveries delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?

Delivered Daily
Daily Newsletter
Sign up for the latest discoveries, groundbreaking research and fascinating breakthroughs that impact you and the wider world direct to your inbox.

Once a week
Life's Little Mysteries
Feed your curiosity with an exclusive mystery every week, solved with science and delivered direct to your inbox before it's seen anywhere else.

Once a week
How It Works
Sign up to our free science & technology newsletter for your weekly fix of fascinating articles, quick quizzes, amazing images, and more

Delivered daily
Space.com Newsletter
Breaking space news, the latest updates on rocket launches, skywatching events and more!

Once a month
Watch This Space
Sign up to our monthly entertainment newsletter to keep up with all our coverage of the latest sci-fi and space movies, tv shows, games and books.

Once a week
Night Sky This Week
Discover this week's must-see night sky events, moon phases, and stunning astrophotos. Sign up for our skywatching newsletter and explore the universe with us!
Join the club
Get full access to premium articles, exclusive features and a growing list of member rewards.
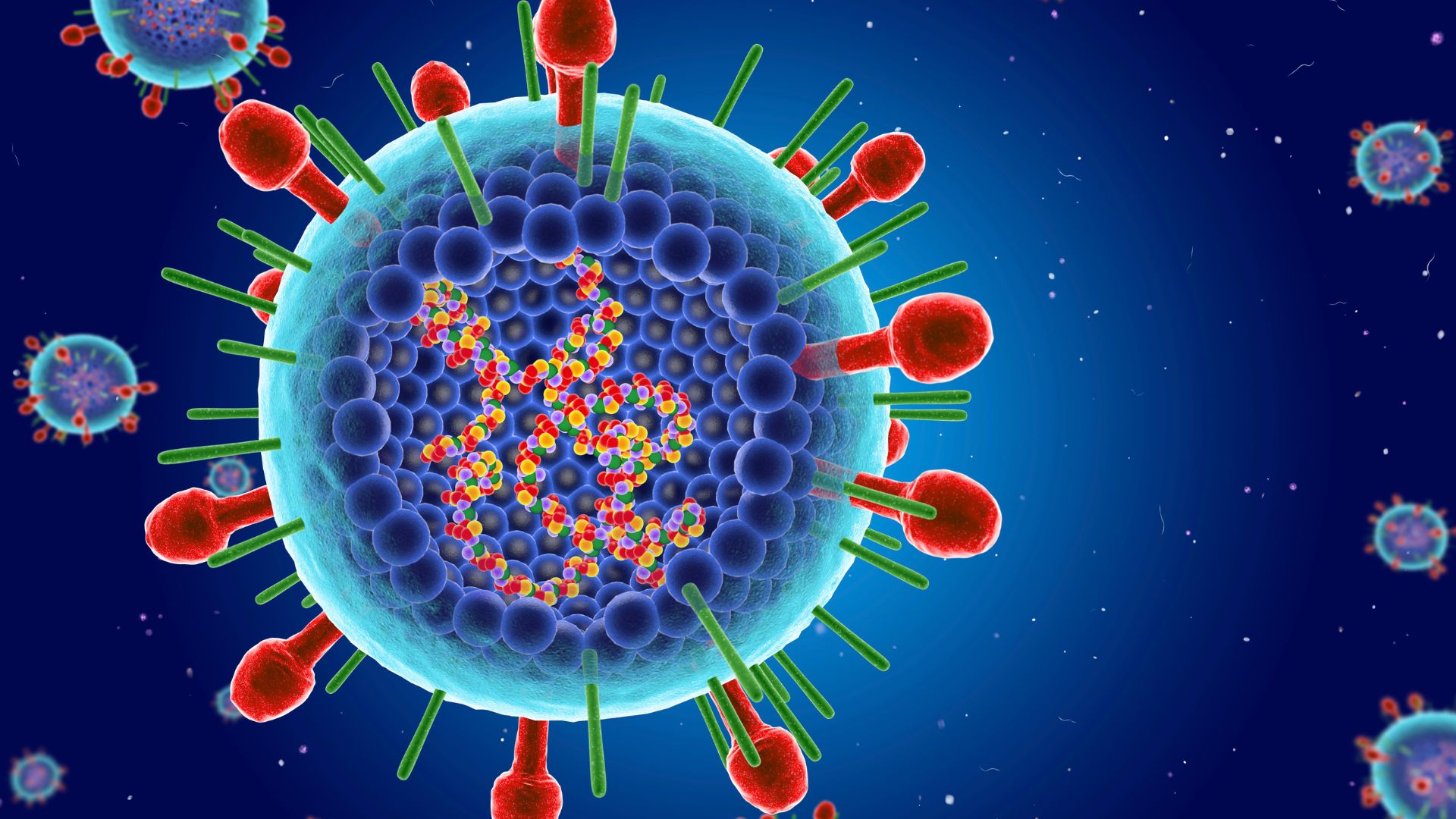
The new RSV vaccines approved for older adults may be linked to a slightly increased risk of a rare neurological condition, a recent analysis finds.
However, the Centers for Disease Control and Prevention (CDC) says the benefits of the vaccines outweigh this slight increased risk. Therefore, the agency still recommends that adults 60 years and older get an RSV vaccine in consultation with their doctor. The available vaccines include one called Arexvy and another called Abrysvo.
The recent research — published May 30 by CDC scientists in the agency's Morbidity and Mortality Weekly Report — is consistent with findings in the clinical trials for the vaccines, according to study leader Anne Hause, an epidemiologist and program lead for V-safe in the CDC's Immunization Safety Office. During clinical trials, researchers observed higher-than-expected rates of Guillain-Barré syndrome, a disorder in which the immune system attacks healthy nerves.
While Guillain-Barré syndrome was noted as a potential concern during the trials, the trials were too small to tease out any possible connection to the shots. Real-world monitoring data involves much larger groups of patients and thus helps confirm the link that trial data hinted at.
Related: Who should get the new RSV vaccines? Here's everything you need to know
Guillain-Barré syndrome causes tingling, numbness and muscle weakness, and it can progress to paralysis. According to the Mayo Clinic, most people recover completely from this illness, but it can take months or years. In severe cases, the condition can affect the muscles that support breathing and be life-threatening.
While Guillain-Barré is fairly rare, RSV, or respiratory syncytial virus, circulates every year and poses a threat to children and older adults, in particular. Among U.S. adults over 65, the seasonal infection kills approximately 6,000 to 10,000 people each year, according to the CDC.
Get the world’s most fascinating discoveries delivered straight to your inbox.
The two new vaccines, one produced by Pfizer and the other by GSK, were approved for older adults in May 2023. The new CDC report examines the first year of safety data using surveys of patients, as well as the Vaccine Adverse Event Reporting System (VAERS), a database where anyone can submit suspected vaccine reactions.
The analysis showed that there were five reports of Guillain-Barré syndrome for every million doses of Pfizer RSV vaccine administered, amounting to 17 cases in total. There were 1.5 reports per million doses of GSK RSV vaccine, or 11 cases in total.
These rates were higher than the background rate of Guillain-Barré expected in this population. This background rate was based on the rates in people given mRNA-based COVID vaccines, which were not tied to any uptick in the syndrome.
However, because VAERS is based on voluntary self-reporting, researchers can't confidently tie every case to the RSV vaccinations, Hause emphasized. Because of this uncertainty, "CDC and FDA are conducting additional safety evaluations in other vaccine safety systems," she said.
Guillain-Barré syndrome often appears after an infection with viruses or bacteria, said Maria Pino, a pharmacologist and associate professor at the New York Institute of Technology's medical school who has written about the RSV vaccines. Similar to the new shots, a 1976 swine flu vaccine was also linked with a slightly increased risk of the syndrome.
The precise link between some infections and vaccinations and the autoimmune syndrome is unknown. However, it likely has something to do with the body's natural immune response to these types of triggers going rogue and turning against the wrong target, Pino told Live Science.
Health officials still recommend getting the RSV vaccines because the risk of developing Guillain-Barré is so low compared with the risk posed by an RSV infection, said Dr. Simon Drysdale, a pediatric infectious disease specialist in the Oxford Vaccine Group. For adults over 60 living in high-income countries, their risk of dying from RSV if they're hospitalized with the infection is 7%, Drysdale said, citing 2023 research published in the journal Influenza and Other Respiratory Viruses.
Unlike the flu or COVID-19, there is no antiviral treatment available for RSV. Rather, treatment involves maintaining a person's vitals in the hope the infection subsides on its own.
"You've got a very, very, very small risk of a significant side effect [from vaccination], versus a much higher risk of having a significant outcome from having RSV disease," Drysdale told Live Science.
For patients deciding whether to get an RSV vaccine, the best source of information is always their own doctor, Pino said. During that discussion, doctors and patients can weigh that specific person's risk factors for RSV complications. Those who face a heightened risk include people with compromised immune function, chronic lung disease and chronic heart disease, as well as those ages 75 and older and those living in long-term care facilities, Hause said.
Other risk factors include frequent contact with children, who carry and spread the virus easily, Drysdale said, as well as chronic kidney disease, which is associated with a high risk of hospitalization from RSV.
"For the vast majority of people," Drysdale said, "the benefit is going to significantly outweigh the risk."
This article is for informational purposes only and is not meant to offer medical advice.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to community@livescience.com with the subject line "Health Desk Q," and you may see your question answered on the website!

Stephanie Pappas is a contributing writer for Live Science, covering topics ranging from geoscience to archaeology to the human brain and behavior. She was previously a senior writer for Live Science but is now a freelancer based in Denver, Colorado, and regularly contributes to Scientific American and The Monitor, the monthly magazine of the American Psychological Association. Stephanie received a bachelor's degree in psychology from the University of South Carolina and a graduate certificate in science communication from the University of California, Santa Cruz.
 Live Science Plus
Live Science Plus










