Scientists develop 'crying' model of human eye tissue
The new model mimics the structure and function of the human conjunctiva in a lab dish, even producing its own tears.

Scientists have created the first 3D model of the human conjunctiva — the clear, protective outer membrane of the eye — in the lab, and it even produces its own tears.
The researchers say the new model could be used to study diseases that affect millions of people, such as conjunctivitis, better known as "pink eye."
The replica conjunctiva is an "organoid" — a lab-grown mass of cells made to resemble 3D, miniature versions of full-size tissues in the body. Organoids are typically grown from stem cells and enable scientists to recreate the structure and function of human organs. Because of this, the models are emerging as promising alternatives to using animals for drug testing.
Until now, there have been no realistic lab models of the human conjunctiva, which has limited research in the field, the scientists behind the new organoid noted. The team reported their findings in a study published Jan. 11 in the journal Cell Stem Cell.
Related: In a 1st, 'minibrains' grown from fetal brain tissue
To make the new model, the study authors collected stem cells from conjunctival tissue provided by organ donors and patients who were undergoing eye surgery. Using chemicals called growth factors, the scientists coaxed the cells into 3D structures that mimicked the human conjunctiva.
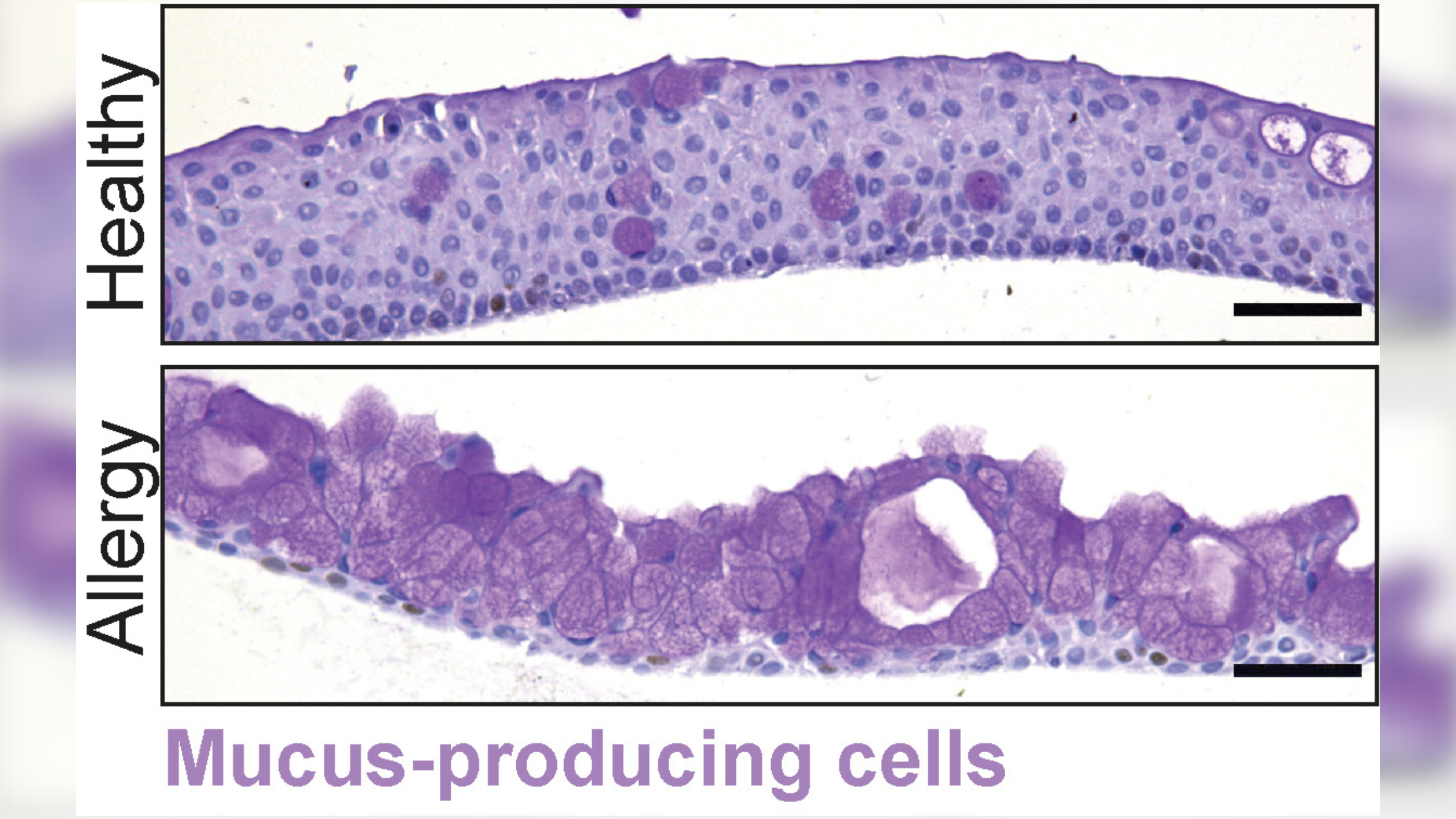
These organoids contained all the cells normally found in the conjunctiva, including mucus-producing cells, such as goblet cells and keratinocytes, which enable the tissue to make mucus-rich tears that protect and lubricate the surface of the eye. However, the study authors found that the latter cells also secreted antimicrobial proteins.
Get the world’s most fascinating discoveries delivered straight to your inbox.
"We discovered that the conjunctiva makes antimicrobial components and therefore contributes to tear production in more ways than by simply making mucus," study first author Marie Bannier-Hélaouët, a postdoctoral researcher in developmental biology and stem cell research at the Hubrecht Institute in the Netherlands, said in a statement.
The new model mimicked all the major features of the human conjunctiva, including its ability to produce mucus-rich tears. In addition to revealing these antimicrobial properties of keratinocytes, the model helped the scientists identify tuft cells, a type of cell not previously known to be in the conjunctiva. These are epithelial cells found in tissues that cover different surfaces of the body and have previously been linked to allergies.
"Similar cells have been discovered in other tissues, but not in the human conjunctiva," Bannier-Hélaouët said.
The authors experimented with the new organoids by applying inflammatory chemicals called interleukins to the models to imitate what would happen during an allergic reaction.
"The organoids started to produce completely different tears: there was more mucus but there were also more antimicrobial components," Bannier-Hélaouët said. The newly discovered tuft cells also became more abundant within the organoid, suggesting they may influence how our eyes respond to allergies, according to the statement.
The authors intend the model to be used to test new drugs to treat diseases of the conjunctiva, including dry eye, which is caused by a poor quantity or quality of tears, and pink eye, or inflammation triggered by an infection, allergies or irritants.
In the study, the researchers infected the organoids with various viruses that are known to cause viral conjunctivitis and then treated the infections with drugs. For example, infection with herpes simplex virus 1, which is mainly responsible for oral and genital herpes but can also cause conjunctivitis, was reversed using antiviral medications.
More research is needed, but the authors hope to one day use this approach to make replacement conjunctivae for people with eye burns, cancer or genetic disorders, according to the statement.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to community@livescience.com with the subject line "Health Desk Q," and you may see your question answered on the website!

Emily is a health news writer based in London, United Kingdom. She holds a bachelor's degree in biology from Durham University and a master's degree in clinical and therapeutic neuroscience from Oxford University. She has worked in science communication, medical writing and as a local news reporter while undertaking NCTJ journalism training with News Associates. In 2018, she was named one of MHP Communications' 30 journalists to watch under 30.
 Live Science Plus
Live Science Plus