A Woman's Odd Symptoms After Chiropractic 'Neck Manipulation' Revealed a Brain Cyst
A women's chiropractic procedure to manipulate her neck may have inadvertently led doctors to discover a large cyst in her brain that had likely been there for decades.
The 22-year-old woman went to the emergency room after experiencing headaches, dizziness and blurred vision for about three months, according to a new report of the case, published online Oct. 5 in The Journal of Emergency Medicine.
Her symptoms began right after she had "cervical spine manipulation," a common chiropractic procedure to treat neck and back pain, as well as other conditions. (In addition to chiropractors, other health practitioners may perform cervical spine manipulation, including physical therapists and osteopathic doctors. In the woman's case, it's unclear who performed the procedure.) [10 Surprising Facts About the Brain]
Because the woman's symptoms began immediately after the cervical spine manipulation, doctors were concerned she may have experienced a complication from the procedure, according to the report. For example, the procedure has been linked to tears in the arteries in the neck, as well as stroke, according to a study published in 2013 in the journal PLOS ONE. But imaging of the woman's neck showed her blood vessels appeared normal.
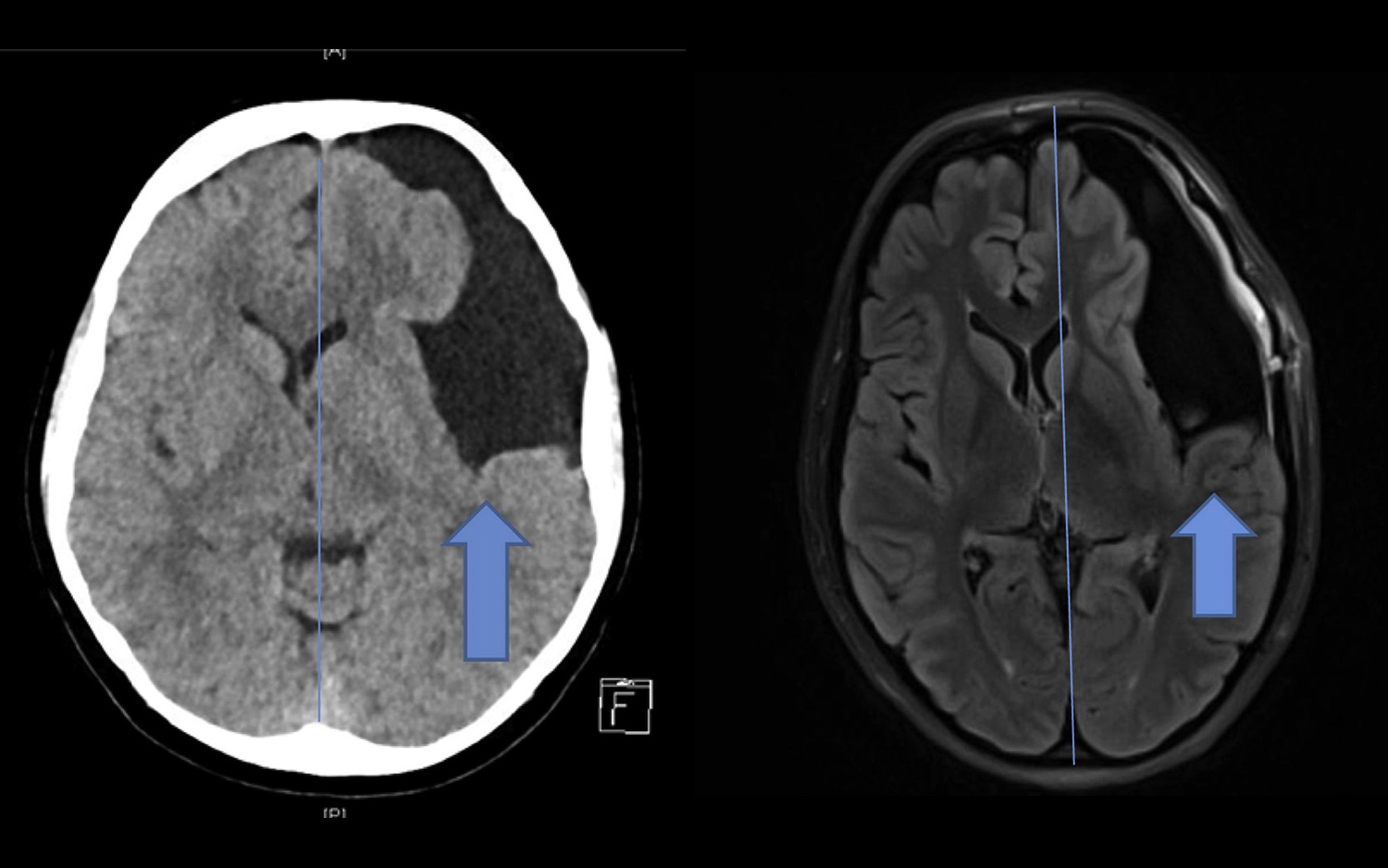
However, a CT scan of her brain showed a large cyst near the front, left side of her head. Specifically, the woman had an arachnoid cyst, a sac filled with cerebrospinal fluid in one of the membranes that covers the brain and spinal cord. These cysts are usually congenital, meaning people have them when they are born. Most people with arachnoid cysts don't have any symptoms; if symptoms do occur, they typically show up in childhood, according to the National Organization for Rare Disorders (NORD).
The new report is the first to link the onset of symptoms from arachnoid cysts with cervical spine manipulation, the authors said. However, the report can't prove that the cervical spine manipulation caused or triggered symptoms from the arachnoid cyst. Instead, it suggests only a possible association between them, said the lead author of the report, Dr. Scott McAninch, an emergency medicine physician at the Baylor Scott & White Medical Center in Temple, Texas.
The goal of the report is to "make other providers around the world aware of the possible association between cervical manipulation [and arachnoid cysts], so that any future cases may be identified," McAninch told Live Science. More cases would suggest a stronger link between the two, McAninch said.
Get the world’s most fascinating discoveries delivered straight to your inbox.
McAninch said his intent is not to criticize cervical spine manipulation, as he supports fair analysis of the procedure's effectiveness in treating symptoms. Instead, it is "to identify a possible unforeseen complication of a practice so that provider and patients can understand [the] risks [and] benefits of said practice, allowing them to make a more informed decision about treatment options," McAninch said.
Most arachnoid cysts don't change in size, and treatment for the cyst may not be necessary if a patient does not have symptoms, according to NORD. But since the woman had symptoms, it was recommended that she undergo surgery that involves opening the cyst to allow the fluid to drain out, McAninch said. After the surgery, the women's symptoms mostly disappeared, the report said.
- 27 Oddest Medical Cases
- 25 Medical Myths That Just Won't Go Away
- 11 Surprising Facts About the Skeletal System
Originally published on Live Science.

Rachael is a Live Science contributor, and was a former channel editor and senior writer for Live Science between 2010 and 2022. She has a master's degree in journalism from New York University's Science, Health and Environmental Reporting Program. She also holds a B.S. in molecular biology and an M.S. in biology from the University of California, San Diego. Her work has appeared in Scienceline, The Washington Post and Scientific American.
 Live Science Plus
Live Science Plus





