The Key to Surviving Superbugs May Be in the Dirt Beneath Our Feet

Get the world’s most fascinating discoveries delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?

Delivered Daily
Daily Newsletter
Sign up for the latest discoveries, groundbreaking research and fascinating breakthroughs that impact you and the wider world direct to your inbox.

Once a week
Life's Little Mysteries
Feed your curiosity with an exclusive mystery every week, solved with science and delivered direct to your inbox before it's seen anywhere else.

Once a week
How It Works
Sign up to our free science & technology newsletter for your weekly fix of fascinating articles, quick quizzes, amazing images, and more

Delivered daily
Space.com Newsletter
Breaking space news, the latest updates on rocket launches, skywatching events and more!

Once a month
Watch This Space
Sign up to our monthly entertainment newsletter to keep up with all our coverage of the latest sci-fi and space movies, tv shows, games and books.

Once a week
Night Sky This Week
Discover this week's must-see night sky events, moon phases, and stunning astrophotos. Sign up for our skywatching newsletter and explore the universe with us!
Join the club
Get full access to premium articles, exclusive features and a growing list of member rewards.
Scientists at Rockefeller University in New York City recently put out a call to citizen scientists: Send us your dirt — literally.
The researchers wanted samples of dirt from across the country that they could probe for naturally occurring compounds that could be turned into drugs.
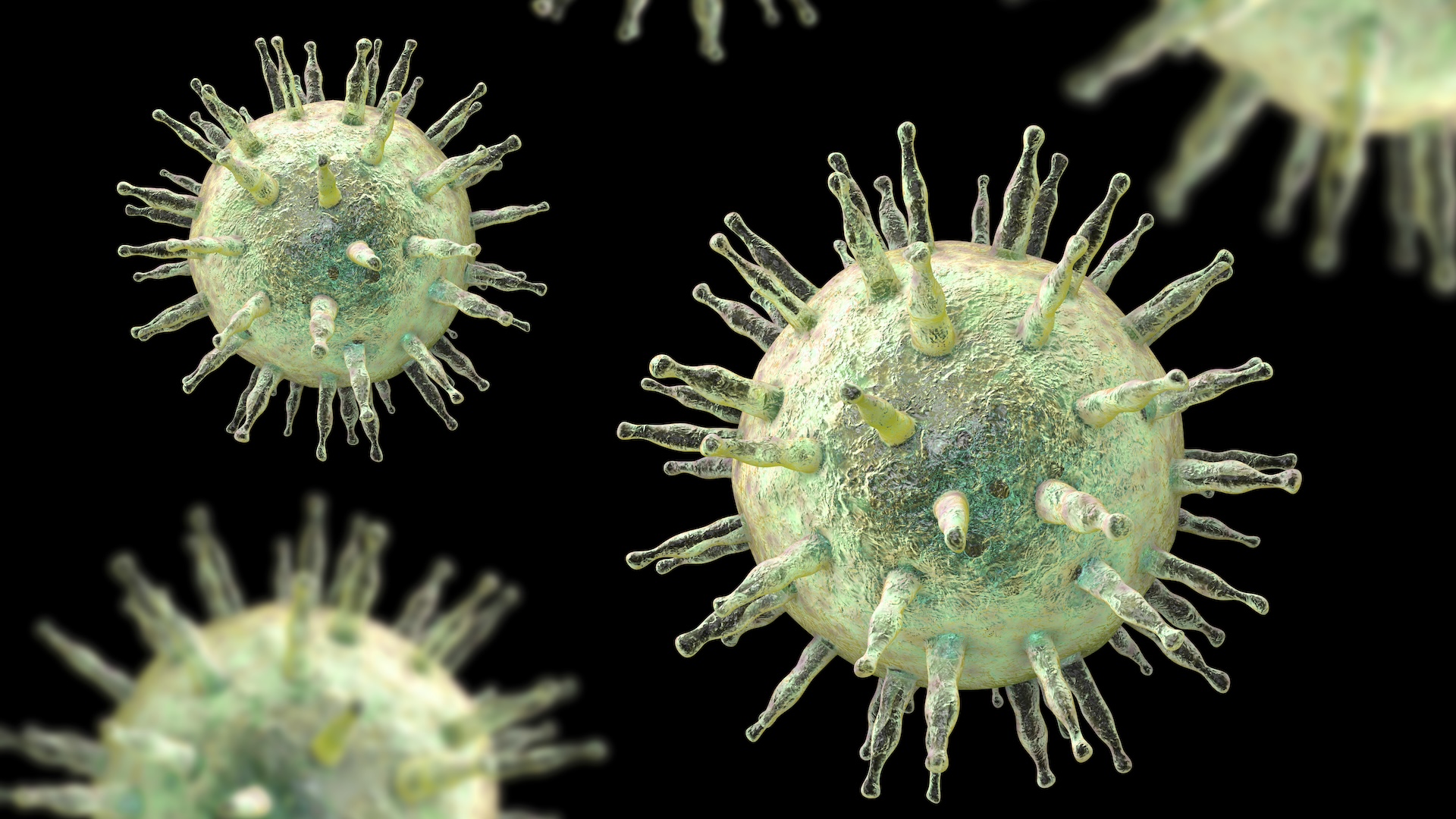
In a new paper, published Feb. 12 in the journal Nature Microbiology, the scientists described the fruits of their labor: a class of antibiotics made by soil-dwelling microbes that may kill deadly superbugs, or bacteria that no longer succumb to known drugs. [6 Superbugs to Watch Out For]
As antibiotic resistance becomes more common, scientists are racing to discover new drugs that can fight these dangerous bacterial infections. (Several of the new study's researchers work for a company called Lodo Therapeutics, whose goal is to discover and develop new drugs.) The antibiotics described in the new study, however, are still years away from being prescribed by doctors — if the medicines even reach that point. Much more research is needed to see if these compounds work in humans.
The antibiotics, called malacidins, are calcium-dependent, meaning they need calcium to be turned "on," according to the study. Malacidins can fight bacteria in different ways, including by attacking bacteria's cell walls. (Human cells don't have walls, so malacidins wouldn't target our cells.)
But how did the researchers sift through nearly 2,000 soil samples to zero in on these microscopic antibiotic-makers?
The scientists knew what they were looking for.
Get the world’s most fascinating discoveries delivered straight to your inbox.
Specifically, the researchers combed through the soil samples for the snippet of genetic code responsible for the "calcium-binding" aspect of the antibiotics — in other words, one of the genes needed to make the malacidins.
After the researchers found these snippets of code in the soil samples, they inserted that DNA into a harmless strain of bacteria, essentially turning the innocuous microbe into a malacidin-making factory.
Then, it was time for the test. Could the malacidin-producing microbes fight off dangerous bacteria?
The researchers applied the microbes to the skin of rats with MRSA-infected wounds. (MRSA, or methicillin-resistant Staphylococcus aureus, is a type of drug-resistant bacteria.) The malacidins appeared to wipe out the MRSA infection, the study found. What's more, the MRSA bacteria didn't appear to develop any type of resistance to the malacidins.
The researchers also looked at how malacidin worked compared with an existing calcium-binding antibiotic called daptomycin. (This drug is used to treat multidrug-resistant infections, the study said). Daptomycin works by disrupting the bacteria cell membrane; experiments in lab dishes showed, however, that malacidin appears to work by targeting not the bacteria cell membrane, but the bacteria cell wall, the researchers said.
Originally published on Live Science.

 Live Science Plus
Live Science Plus