What Is MRSA?
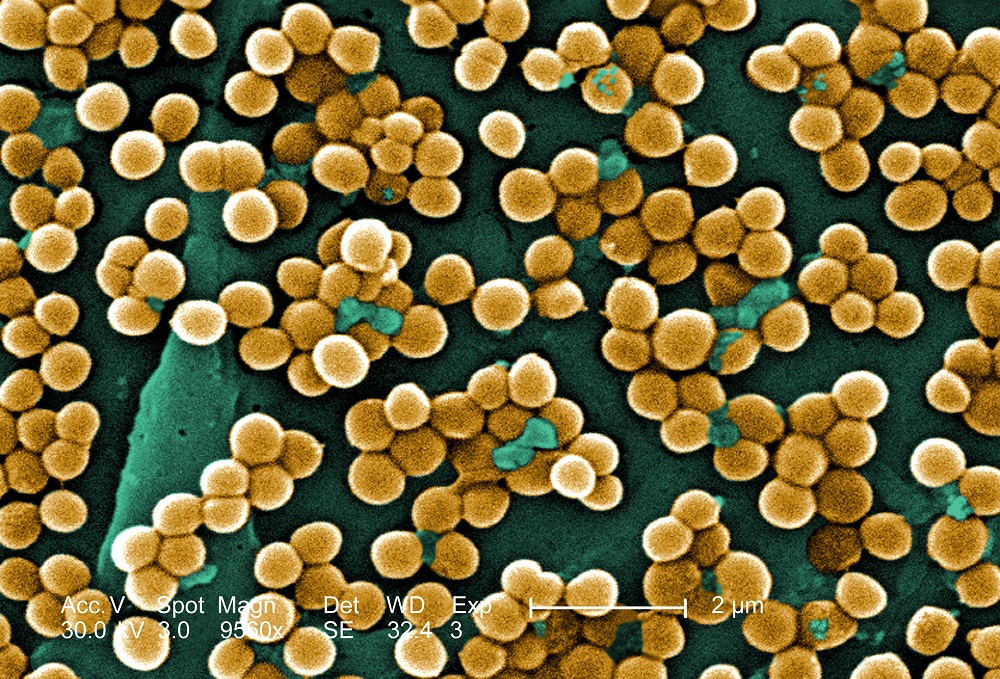
Methicillin-resistant Staphylococcus aureus, or MRSA, is a strain of staph bacteria that is resistant to the antibiotics normally used to treat such infections.
In the 1940s, some 60 years after the discovery of the bacterium S. aureus, doctors began treating staph infections with penicillin. But the overuse and misuse of the drug helped the microbes evolve with resistance to penicillin by the 1950s.
Doctors then started using methicillin to counter the growing problem of penicillin-resistant staph infections, and the new drug quickly became the common treatment for S. aureus, according to the National Institute of Allergy and Infectious Diseases.
In 1961, British scientists discovered MRSA; the first case of this "superbug" in the United States occurred in 1968. Over time, strains of MRSA developed resistances to other penicillin-related antibiotics.
In fact, MRSA is now resistant to an entire class of penicillin-like antibiotics called beta-lactams, which includes amoxicillin, oxacillin, dicloxacillin and many others.
Experts used to think MRSA only affected people in health care settings, particularly patients with weakened immune systems or those who had recently undergone surgery. But in the 1990s, a different strain of MRSA emerged outside of the hospital. This "community-associated MRSA" predominantly affects people who are frequently in close, physical contact with others, such as athletes, inmates, soldiers and childcare workers.
Today it's quite common — and normal — to have staph bacteria on your skin or in your nose. Indeed, about one-third of the world's population have S. aureus bacteria on their bodies, and about 2 percent of people carry MRSA, according to the Centers for Disease Control and Prevention.
Get the world’s most fascinating discoveries delivered straight to your inbox.
Usually, the staph on a person's skin doesn't cause an infection or disease symptoms, but problems can arise if the bacteria gets into the body. Staph skin infections start off as a small, red bump that resembles a spider bite — these infections can progress quickly, turning into swollen, painful abscesses, which doctors need to surgically drain.
If the bacteria burrow deeper, they can cause infections throughout the body, including in the bloodstream, heart, bones, joints, lungs and surgical wounds, which can result in chest pain, fever and even death.
As a last resort, life-threatening MRSA infections can still be treated with the antibiotic vancomycin. However, new treatments may eventually be needed, as a few cases of vancomycin-resistant S. aureushave already been reported.
Follow Joseph Castro on Twitter. Follow us @livescience, Facebook & Google+.



