A Revolution in Breast Cancer Treatment? Milder Options are Emerging (Op-Ed)


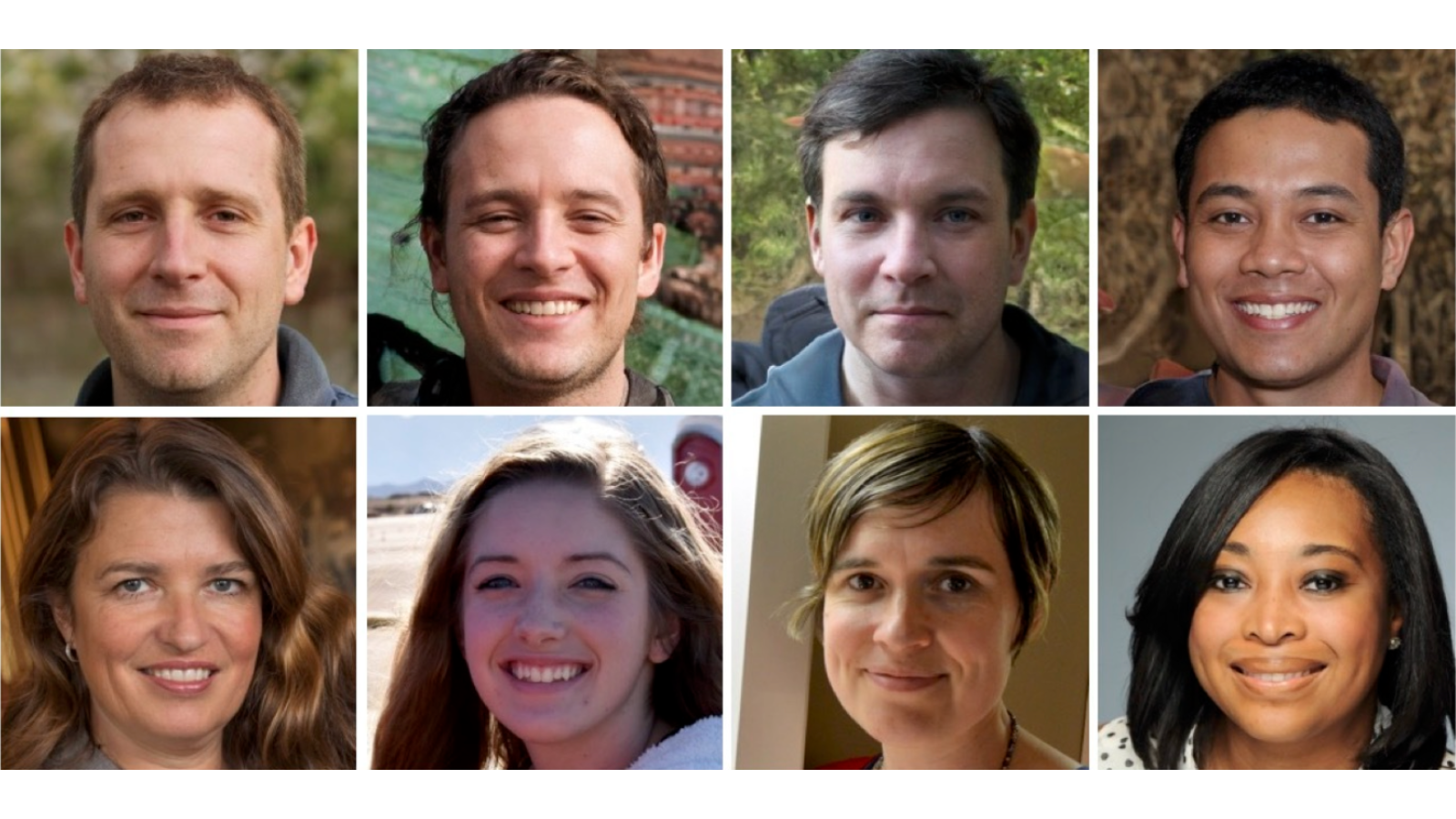
Dr. Bhavesh Balar, oncologist and hematologist; Dr. Amit Kharod, general surgeon and chief of the Department of Surgery at CentraState Medical Center; Dr. Mary Martucci, breast surgeon; and Dr. Kenneth Tomkovich, interventional radiologist, are on staff at the Statesir Cancer Center at CentraState Medical Center in Freehold, N.J. They contributed this original article to Live Science's Expert Voices: Op-Ed & Insights.
In just the past decade, there has been a rapid evolution in breast cancer diagnosis and treatment protocols. As a result, therapy today is less invasive and far more effective than in the late '90s, when mastectomy and lumpectomy were considered the gold standard for care.
Not only are we discovering the majority of cancers in earlier stages (0-1), but also the five-year breast cancer survival rate is nearly 90 percent today. However, with more than 230,000 women expected to be diagnosed in the United States with breast cancer this year alone, treatment options will play a pivotal role in saving lives.
While breast cancer is far from the death sentence it once was, it is still nonetheless challenging to treat.
Breast cancer, disguised
Researchers have learned that breast cancer is not one, singular disease. Rather, breast cancer's cell biology is composed of many subtypes of different kinds of cancer that act — and react — differently in every patient. The more oncologists learn about each subtype, the better they can effectively treat tumors and keep cancer cells from spreading.
Studies today are focusing on understanding the molecular makeup of different types of breast cancer. Thanks to advances in genomic testing and deeper insights into the biology of these subtypes, doctors no longer use the one-size-fits-all approach.
Get the world’s most fascinating discoveries delivered straight to your inbox.
Every cancer patient has a different profile of biological risk. Once that risk profile is identified through genetic testing, the attending oncological team uses this unique data to create a personalized treatment and preventative plan for the patient. This allows us to achieve the most promising outcome for the individual, based specifically on her DNA.
Many breast cancers are slow-growing tumors that may never cause symptoms or even threaten to shorten a patient's life span. Conversely, other breast cancers spread very aggressively, even before they are diagnosed. [US Breast Cancer Cases May Rise 50 Percent by 2030 ]
Breast cancer in stages 0 to 3 becoming a treatable disease
Looking ahead to the next five years, earlier-stage breast cancer (stages 0-3) therapy will continue to evolve, making this a more treatable disease when diagnosed in the earlier In fact, earlier-stage cancers may not be treated with surgery at all.
Early cancer staging indicates the size of the tumor and/or abnormal cells, and whether or not those cells are still contained to the place of origin:
Stage 0: Atypical cells are non-invasive and have not spread outside milk ducts or lobules into the surrounding breast tissue. Stage 1: Cancer is evident, but confined to the area where the first abnormal cells began to develop. Stage 2: Cancer is growing, but still contained in the breast or nearby lymph nodes. Stage 3: Cancer has extended beyond the immediate region of the tumor, may have invaded nearby lymph nodes and muscles, but has not metastasized into additional organs.
Beating a cancer cell at its own game
Cancer is a collection of irregular cells that grow in the body, largely ignored by the immune system and its efforts to overcome and kill invasive cellular matter. One of the most frustrating mysteries that has plagued researchers is why the body allows this to happen when it successfully fights off cold, flu and other foreign cellular combatants every day.
We now know that cancer cells are shielded by a transmembrane protein barrier, called programmed death-ligand 1 (PD-L1), which suppresses the immune system in much the same way as during a pregnancy, allowing cells to multiply and grow unabated.
But cancer researchers are conducting promising clinical trials on patients who have metastatic breast cancer. These researchers use a cocktail of intravenous "inhibitor" drugs that remove the protective cancer-cell shield and enable the immune system to do its job. As a result, the medication empowers the patient's own defenses to kill the cancer cells, offsetting their ability to grow and spread. These drugs work by basically removing the brakes from the body's immune system. However, it is important to note that sometimes the immune system starts attacking other parts of the body, which can cause serious, or even life-threatening, problems in the lungs, intestines, liver, hormone-making glands, kidneys or other organs.
It's also important to note that these drugs are not chemotherapy; rather, they are an innovative immunotherapy that targets tumors and is markedly less harmful to patients.
Similar trials were previously conducted to combat melanoma, bladder cancer and lung cancer, and these tests have yielded positive results.
This drug protocol holds tremendous promise for the treatment of all kinds of cancers. It has the potential to revolutionize the way we treat people who have been diagnosed with any kind of cancer. (Side effects from these drugs can include fatigue, cough, nausea, itching, skin rash, decreased appetite, constipation, joint pain and diarrhea.)
Targeting immune system checkpoints is quickly becoming an important part of treatment for some cancers, such as melanoma and lung cancer. Unlike other cancer drugs, these checkpoint inhibitors seem to be helpful against many different types of cancer. Only a few of these treatments have been approved for use so far, but others are now being evaluated in clinical trials. Overall, it offers additional options for treatment; it remains to be seen if it would replace current chemotherapy in certain types of cancers or if it would complement existing treatments for other cancers.
Surgery will be less common and less invasive
Surgery has traditionally been the first treatment protocol after a breast cancer diagnosis. Not so long ago, a woman with a suspicious lump went into surgery with no idea if she would awaken without a breast.
As breast cancer specialists, we see our jobs changing significantly down the road. We will continue to use fewer and fewer invasive procedures to fight cancer of the breast. And, if all goes well, most of us should be out of a job at some point.
In the future, breast surgeons may see their role evolve into a more educational one — working with patients and health care providers to help those affected make the right choices for their particular situations.
These less-invasive surgical approaches not only cause less trauma to women, but they also achieve outcomes comparable to previous, more-invasive surgeries. For example, a 20-year study showed that women with early stage breast cancer (stage 0-2) who underwent mastectomies (breast removal) had about the same prognosis and cancer-recurrence rates as women who underwent breast-conserving lumpectomy (removing only the tumor and an area of surrounding tissue).
Still, today, the health care community is not completely up to speed on newer treatment options. It's the job of breast cancer physicians to educate other health care professionals, along with patients and families, about the myriad treatment, preventive and diagnostic choices available.
Disintegrating smaller breast cancers without surgery
One of us at Statesir Cancer Center, interventional radiologist Dr. Kenneth Tomkovich, is co-principal investigator overseeing a promising national clinical research trial that uses a cell-freezing technique called cryoablation. This method can extinguish breast tumors no larger than 1.5 centimeters (0.6 inches).
Cryoablation has been previously tested and approved to treat liver, prostate, kidney, skin and cervical cancer. Testing this technique to treat tumors in the breast was a logical follow-up.
Today, women are more diligent about getting routine mammograms and performing self-care exams, and this helps physicians catch more cancers in earlier stages. Our research trial hopes to confirm that freezing these small breast tumors — in lieu of surgically removing them — is less invasive for the patient but ultimately yields comparable long-term patient outcomes against cancer recurrence.
Compared to traditional surgery, cryoablation is less risky and more cost-effective; it also offers faster recovery and improved cosmetic results, resulting in greater patient comfort.
The nationwide trial includes women age 65 and older. That's because patients in this age group often have additional health issues, such as heart or lung disease, that make them poor candidates for the rigors of traditional breast surgery. While these trial participants were also offered chemotherapy and radiation in lieu of surgery, those treatments come with significant short- and long-term side effects.
Breast cryoablation is similar to a needle biopsy procedure, which is performed in the doctor's office under local anesthesia.
Using ultrasound guidance, an FDA-approved cryoprobe (thin needle) is inserted until it reaches the center of the tumor. Liquid nitrogen, chilled to minus 160 degrees Celsius (minus 256 degrees Fahrenheit), is injected into the center of the tumor. The goal is to kill the cancerous tumor, along with a thin rim of normal tissue surrounding it, to ensure that the cancer is fully treated (i.e., frozen).
According to trial patients, there are few unpleasant side effects with this treatment, and the patient can go home immediately after the procedure. Over the course of several months, the tumor gradually dissolves away.
While long-term outcomes will be studied in years to come, we anticipate cancer-recurrence rates comparable to those of traditional surgical tumor removal. This forecast is based upon longer-term outlooks from previous patients who have undergone cryoablation therapy for other types of cancer.
Cancer treatment no longer means just calling a breast surgeon
The diagnostic focus of breast cancer is still centered on staging, but now includes a molecular evaluation of the tumor as well. These priorities take precedence over more-traditional markers such as the size of the tumor or whether it has entered the lymph nodes or other parts of the body.
Additionally, the days of receiving a cancer diagnosis and automatically assuming one will lose the breast are certainly over.
Physicians can now manage this disease so differently because current treatment options are so plentiful. The cancer treatment community now concentrates on the staging and molecular (genetic) makeup of the tumor first and foremost. After this is determined, the patient partners with a cancer team — medical oncologist, breast surgeon, radiation oncologist and holistic therapy professionals — who collectively devise a multipronged treatment strategy. This is an improved method for fighting cancer that is still big news to a large part of the public.
Follow all of the Expert Voices issues and debates — and become part of the discussion — on Facebook, Twitter and Google+. The views expressed are those of the author and do not necessarily reflect the views of the publisher. This version of the article was originally published on Live Science.