Cells in Living Mice 'Reprogrammed' to Embryonic-like State
Get the world’s most fascinating discoveries delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?

Delivered Daily
Daily Newsletter
Sign up for the latest discoveries, groundbreaking research and fascinating breakthroughs that impact you and the wider world direct to your inbox.

Once a week
Life's Little Mysteries
Feed your curiosity with an exclusive mystery every week, solved with science and delivered direct to your inbox before it's seen anywhere else.

Once a week
How It Works
Sign up to our free science & technology newsletter for your weekly fix of fascinating articles, quick quizzes, amazing images, and more

Delivered daily
Space.com Newsletter
Breaking space news, the latest updates on rocket launches, skywatching events and more!

Once a month
Watch This Space
Sign up to our monthly entertainment newsletter to keep up with all our coverage of the latest sci-fi and space movies, tv shows, games and books.

Once a week
Night Sky This Week
Discover this week's must-see night sky events, moon phases, and stunning astrophotos. Sign up for our skywatching newsletter and explore the universe with us!
Join the club
Get full access to premium articles, exclusive features and a growing list of member rewards.
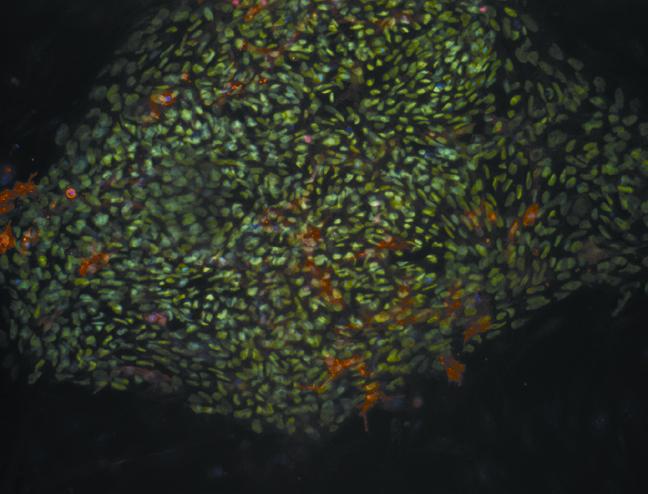
Cells in a living animal can be reprogrammed into a more primitive, embryonic-like state, in which they are capable of transforming into any cell in the body, a new study finds.
Such cells, known as induced pluripotent stem cells (iPS), have been created before, but only by using lab dishes to grow them. The new study is the first to turn back the developmental clock on cells while they are inside a living organism — in this case, a mouse.
Interestingly, the researchers said, the iPS cells created in mice in the study appear to be in a more primitive state than those created in lab dishes, meaning that the former could be able to transform into a more diverse set of tissues. [Stem Cells: 5 Fascinating Findings]
It will likely be many years before the new findings have any application for people, the researchers said. (In fact, the mice in the study developed many tumors.) Still, the findings open up new possibilities for regenerative medicine, said study researcher Manuel Serrano, director of the Molecular Oncology Program at the Spanish National Cancer Research Center.
Currently, iPS cells created in a lab dish need to be engrafted, or reintegrated, back into the body — a very inefficient process, Serrano said. But by generating iPS cells within the body, "The cells have already integrated into the tissue; they are already there, in the right position," Serrano said at a news conference about the study, which is published in the Sept. 12 issue of the journal Nature.
The researchers now need to determine whether iPS cells created in a living organism are capable of regenerating damaged tissue — a key step in determining their therapeutic potential.
Creating stem cells
Get the world’s most fascinating discoveries delivered straight to your inbox.
Embryonic stem cells can give rise to virtually any cell type in the body, such as skin or heart cells, so they are being investigated for their ability to treat illnesses. However, embryonic stem cells exist during only the first days of an embryo's development, so they cannot be found in adults.
In 2006, Shinya Yamanaka of Kyoto University in Japan showed that, by adding only four genes, adult cells in a lab dish could be transformed into embryoniclike cells, so these cells were given the name "induced pluripotent stem cells." (Last year, Yamanaka received a Nobel Prize for the work.)
In the new study, Serrano and his colleagues achieved the same feat, but they didn't use a lab dish. The researchers created "reprogrammable mice," or genetically engineered mice in which the four genes found by Yamanaka could be "turned on" by a "switch." The switch, in this case, was exposure to a drug called doxycycline (an antibiotic).
When the mice drank water spiked with doxycycline, they developed teratomas in various tissues. Teratomas are tumors that originate from pluripotent cells, and contain the three main groups of cells formed during embryo development, although they are disorganized. The presence of teratomas in the mice indicated that the researchers had, indeed, turned back the clock on the mouse tissue cells.
When the researchers further analyzed the iPS cells that formed in the mice, they found that the cells had the ability to differentiate into not only body tissues, but also cells that form the placenta. Human embryos have this capability when they are 72 hours old, but it has never been replicated in a laboratory.
"This data tell us that our stem cells are much more versatile" than those created in a lab dish, the researchers said.
Therapeutic potential
The new finding "calls into question what it really means for a cell to be completely reprogrammed. You can no longer just say an iPS cell has been reprogrammed," said Dr. Robert Lanza, chief scientific officer at biotech company Advanced Cell Technology.
Figuring out what it means for a cell to be "truly reprogrammed" may help researchers improve reprogramming of human cells in a laboratory, and perhaps understand why some iPS cells made in lab dishes haven't been working as well as researchers would like, Lanza said.
However, the approach used in the new study with "reprogrammable mice" obviously is not applicable or testable in people, Lanza said.
The researchers said an approach in people might use a harmless virus to introduce certain genes that could perhaps be turned off with a "switch," as was done in the study with mice. A safety obstacle would be to make sure the approach did not cause teratomas to develop.
The first clinical trial to attempt to test lab-made iPS cells in people was approved in Japan in July, and aims to turn skin cells into retinal cells to treat age-related macular degeneration, which causes blindness.
The researchers of the new study noted that it took seven years from the discovery of iPS cells to begin the first clinical trial on people, and speculated that a similar amount of time may need to pass before in vivo iPS cells could be tested in people.
Follow Rachael Rettner @RachaelRettner. Follow LiveScience @livescience, Facebook & Google+. Original article on LiveScience.

Rachael is a Live Science contributor, and was a former channel editor and senior writer for Live Science between 2010 and 2022. She has a master's degree in journalism from New York University's Science, Health and Environmental Reporting Program. She also holds a B.S. in molecular biology and an M.S. in biology from the University of California, San Diego. Her work has appeared in Scienceline, The Washington Post and Scientific American.
 Live Science Plus
Live Science Plus










