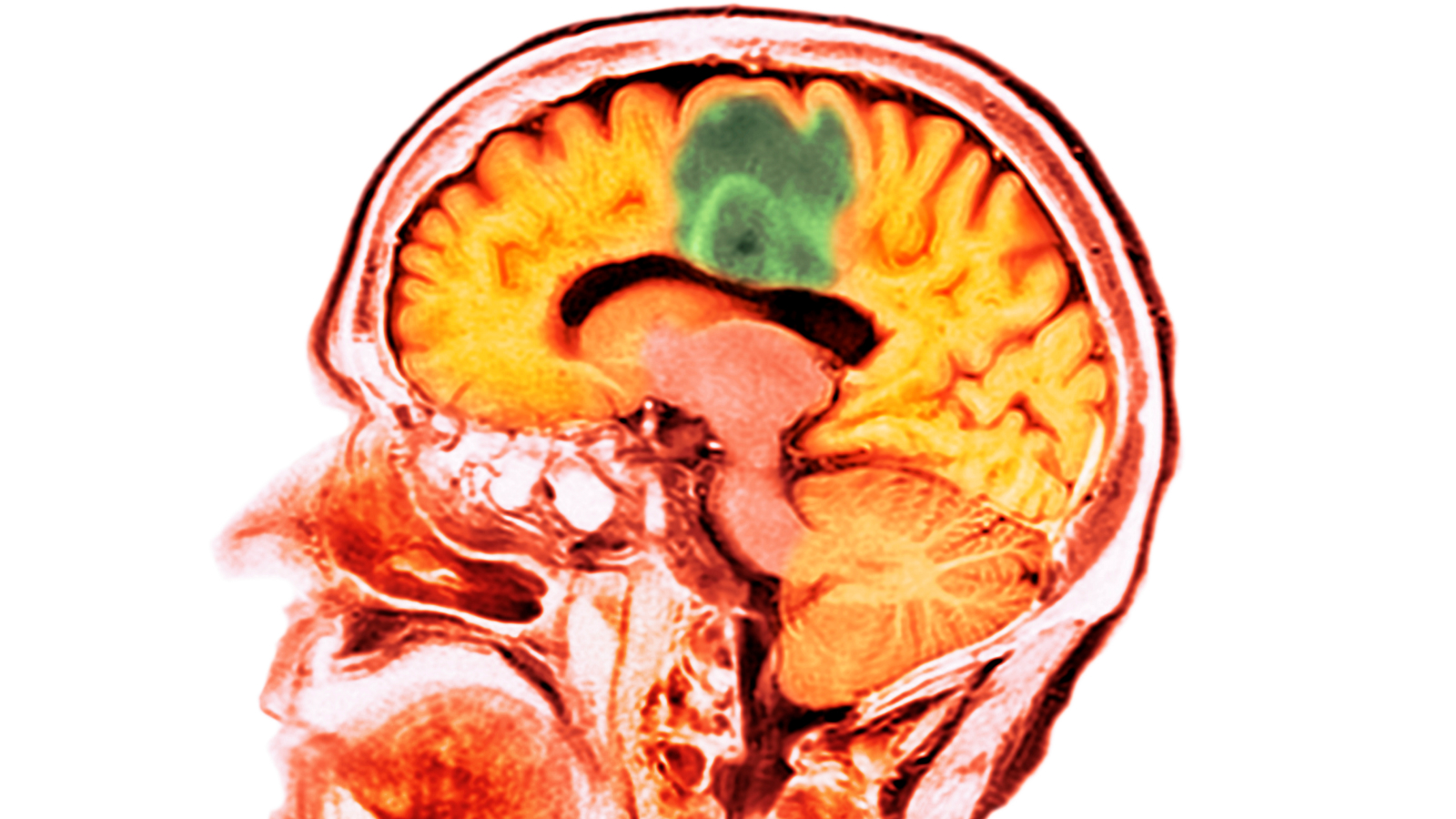
New mRNA vaccine for deadly brain cancer triggers a strong immune response
COVID-19 vaccine development paves way to a new class of cancer immunotherapy.
Get the world’s most fascinating discoveries delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?

Delivered Daily
Daily Newsletter
Sign up for the latest discoveries, groundbreaking research and fascinating breakthroughs that impact you and the wider world direct to your inbox.

Once a week
Life's Little Mysteries
Feed your curiosity with an exclusive mystery every week, solved with science and delivered direct to your inbox before it's seen anywhere else.

Once a week
How It Works
Sign up to our free science & technology newsletter for your weekly fix of fascinating articles, quick quizzes, amazing images, and more

Delivered daily
Space.com Newsletter
Breaking space news, the latest updates on rocket launches, skywatching events and more!

Once a month
Watch This Space
Sign up to our monthly entertainment newsletter to keep up with all our coverage of the latest sci-fi and space movies, tv shows, games and books.

Once a week
Night Sky This Week
Discover this week's must-see night sky events, moon phases, and stunning astrophotos. Sign up for our skywatching newsletter and explore the universe with us!
Join the club
Get full access to premium articles, exclusive features and a growing list of member rewards.
For the first time, scientists have tested a messenger RNA (mRNA) vaccine in a patient with a deadly form of brain cancer — and it triggered a strong immune response.
The vaccine, which was described in a study published on May 1 in the journal Cell, was created by extracting genetic material called RNA from a tumor from a patient with glioblastoma, an aggressive type of cancer. The RNA was then replicated to make a vaccine from mRNA, which is a blueprint for what is inside every cell, including tumor cells.
"These results represent an exciting advance in next generation cancer therapies that leverage mRNA, the same class of medicines used in the COVID-19 vaccines," Owen Fenton, an assistant professor of pharmacoengineering and molecular pharmaceutics at the University of North Carolina at Chapel Hill, who was not involved in the study, told Live Science in an email.
Moving at the speed of cancer
People have been developing cancer vaccines, or treatments that boost the body’s immune system attack against cancer cells, since the 1800s. However, cancer vaccines rarely mount an immune response strong enough to overcome the cancer.
Cancers mutate rapidly, so if doctors cut out a tumor and do a biopsy, the tumor itself may be different within 24 hours, said study senior author Dr. Elias Sayour, a pediatric oncologist and associate professor of neurosurgery at the University of Florida.
And by the time immune therapy begins, “the cancer is out of control now and so now the immune response is like a water gun in the face of a forest fire," Sayour told Live Science.
Up until now, cancer vaccines being tested have aimed to mount an immune response to a small number of molecular signatures from tumors from many different patients. In clinical trials, the vaccine material is often packaged into tiny lipid nanoparticles, but the trials typically only deliver a small number of particles and the vaccines themselves take months, if not years, to develop. However, cancer cells can adapt very quickly, figuring out ways to disable or block recognition by the local immune system.
Get the world’s most fascinating discoveries delivered straight to your inbox.
By isolating all the mRNA signatures in a patient’s tumor, designing a larger lipid nanoparticle and delivering more of the mRNA particles at once, Sayour and his team demonstrated an aggressive immune response specific to the patient’s tumor. And because mRNA can be isolated, amplified, and packaged for delivery within a matter of days, these tailored vaccines can be generated in about a month.
Sayour and other researchers hypothesize that the larger payload makes the nanoparticle look more dangerous to the body’s immune system, mounting a larger response.
And by using the vaccine technology developed against the COVID-19 virus, Sayour and his team were able to quickly create a vaccine specific to one patient’s tumor and train the patient’s immune system to specifically attack the tumor before it changed.
"The beauty of RNA, which I think was proven in [the COVID-19] vaccines, is you can update them quickly and keep up against the spread of the pandemic. What if we could do the same in cancer?" said Sayour.
This novel therapy could likely be tailored to mount an immune response against other tumors in conjunction with existing therapies.
However, the study is still in very early days. As with all immunotherapies, there is a risk of an out-of-control immune response.
Sayour and his team will soon be treating more people in an expanded clinical trial to hone in on a treatment dosage that could minimize the harmful effects of a strong immune response and to see if the targeted mRNA vaccine works in other patients.

Jennifer Zieba earned her PhD in human genetics at the University of California, Los Angeles. She is currently a project scientist in the orthopedic surgery department at UCLA where she works on identifying mutations and possible treatments for rare genetic musculoskeletal disorders. Jen enjoys teaching and communicating complex scientific concepts to a wide audience and is a freelance writer for multiple online publications.
 Live Science Plus
Live Science Plus










