How a Man's Fecal Transplant Turned Fatal
A 73-year-old man is the first person known to die as a result of the procedure.
The first person known to die as a result of a fecal transplant is a 73-year-old man who developed a fatal infection with antibiotic-resistant bacteria that were in the donor's stool sample.
News of the man's death surfaced in June; he was one of two patients in separate clinical trials who became ill after receiving fecal transplants from the same donor, Live Science previously reported.
Both patients developed infections with a strain of Escherichia coli, or E. coli, that demonstrated resistance to different types of antibiotics. Details of the man's death were described in a new study published online yesterday (Oct. 30) in The New England Journal of Medicine.
Related: 5 Ways Gut Bacteria Affect Your Health
The two patients, who were participants in clinical trials conducted at Massachusetts General Hospital (MGH), received fecal transplants in the form of pills that were made in November 2018.
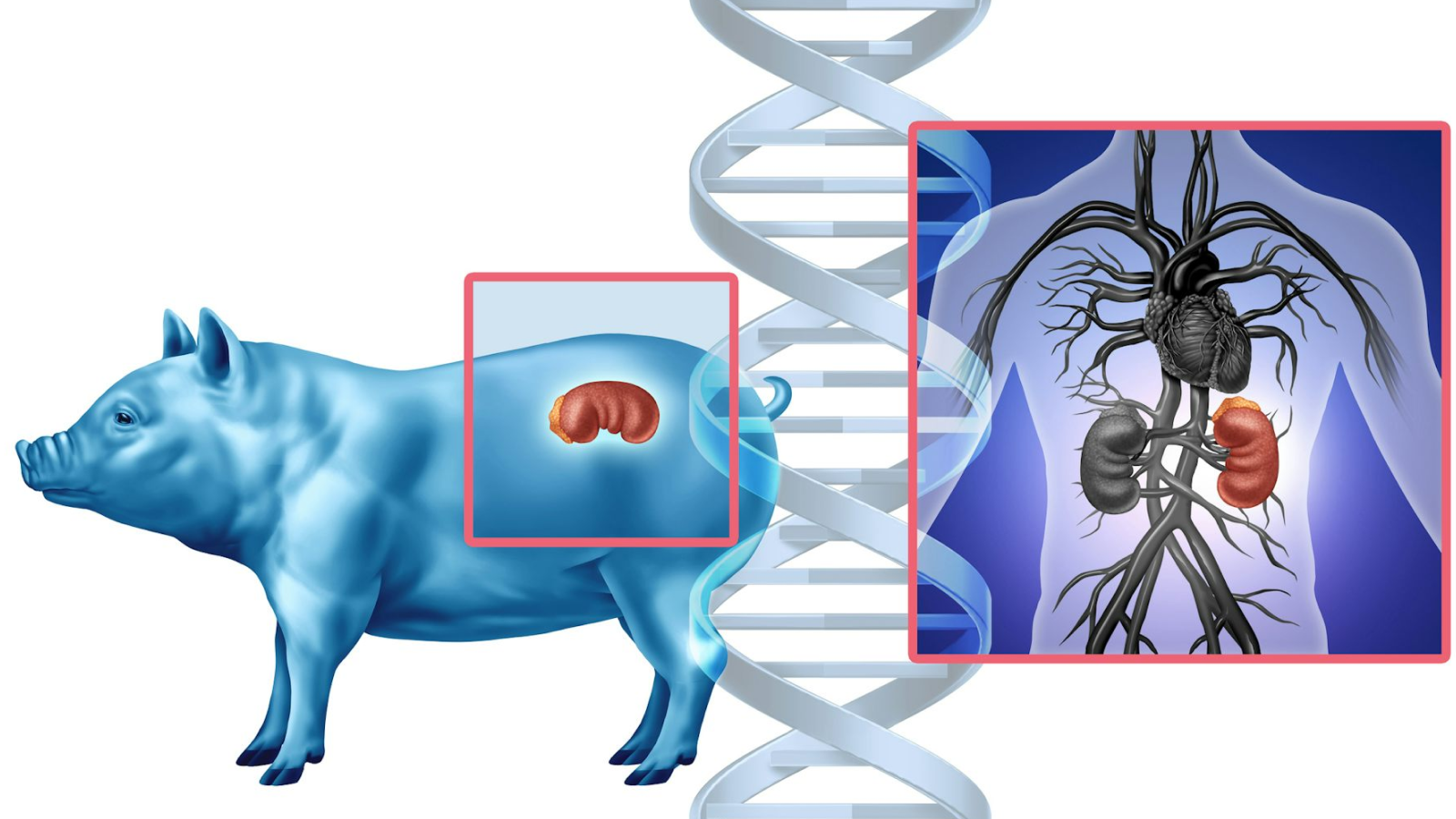
Fecal microbiota transplantation (FMT) — commonly known as a "poop transplant" or fecal transplant — is emerging as an effective experimental treatment for Clostridium difficile, or C. diff, a potentially life-threatening bacterial gut infection. In guts with depleted microbial diversity, poop transplants boost diversity with microbial infusions from a healthy person's gut microbiome, distilled from stool samples and delivered as an enema or an oral pill.
But FMT is also being tested as a method of restoring gut microbial diversity for conditions not caused by C. diff. The two clinical trials at MGH were testing the impact of FMT on microbiome issues associated with liver disease and the effectiveness of preventive FMT prior to stem cell transplants.
Get the world’s most fascinating discoveries delivered straight to your inbox.
Eight days after the 73-year-old patient received his last FMT dose, he developed a fever and chills, and exhibited "altered mental status," according to the study. His condition quickly worsened. The man developed sepsis — an extreme immune response to infection causing inflammation throughout the body and organ damage — and died two days later, with evidence of an antibiotic-resistant strain of E. coli in his blood.
The other patient who became ill from the FMT, a 69-year-old man, also tested positive for the drug-resistant strain of E. coli. However, his infection responded to treatment with antibiotics. Eventually, he was pronounced "clinically stable," the researchers wrote in the study.
Antibiotic resistance in harmful bacteria is a growing concern worldwide. With the emergence of these so-called superbugs — some of which can share their resistance with other bacteria — entire classes of antibiotics are becoming less effective at quelling infections, and health practitioners are losing key weapons in their disease-fighting arsenals.
High-risk patients
In January 2019, a regulatory review by the U.S. Food and Drug Administration (FDA) dictated that stool samples for FMT had to be screened for drug-resistant microbes. But as this E. coli strain is rare in healthy people, the pills that were produced in November were not tested retroactively, the study authors reported.
Both of the FMT-sickened patients were considered at high risk for bacterial infection because of conditions that weakened their immune systems. The man who recovered had advanced cirrhosis — severe scarring of the liver — and the man who died had recently undergone a stem cell transplant and was taking immunosuppressing drugs so that the transplant would not be rejected, the scientists reported. Samples from the same donor were administered to 22 patients in all, and although several other recipients tested positive for the resistant E. coli, the bacteria didn't make them ill.
On Nov. 4, FDA officials will conduct a 7-hour public hearing at the agency's Silver Spring, Maryland, campus, "to obtain public input on the state of the science regarding FMT to treat C. difficile infection not responsive to standard therapies," according to a notice on the FDA website.
The FDA hearing will also review clinical evidence to evaluate the effectiveness and risks of using FMT to combat persistent C. difficile "and to better understand the impact of FDA's enforcement policy on product development," agency officials said in the statement.
- The Poop on Pooping: 5 Misconceptions Explained
- Microbiome: 5 Surprising Facts About the Microbes Within Us
- 8 Tips to Be a Probiotic Pro
Originally published on Live Science.

Mindy Weisberger is a science journalist and author of "Rise of the Zombie Bugs: The Surprising Science of Parasitic Mind-Control" (Hopkins Press). She formerly edited for Scholastic and was a channel editor and senior writer for Live Science. She has reported on general science, covering climate change, paleontology, biology and space. Mindy studied film at Columbia University; prior to LS, she produced, wrote and directed media for the American Museum of Natural History in NYC. Her videos about dinosaurs, astrophysics, biodiversity and evolution appear in museums and science centers worldwide, earning awards such as the CINE Golden Eagle and the Communicator Award of Excellence. Her writing has also appeared in Scientific American, The Washington Post, How It Works Magazine and CNN.