An immunologist explains why the immune system works best when balanced, not 'boosted'
Disease can arise both when immune cells are too active and when they're not active enough.
For immune health, some influencers seem to think the Goldilocks philosophy of "just right" is overrated. Why settle for less immunity when you can have more? Many social media posts push supplements and other life hacks that "boost your immune system" to keep you healthy and fend off illness.
However, these claims are not based on science and what is known about immune function. Healthy immune systems don't need to be "boosted." Instead, the immune system works best when it is perfectly balanced. Scientific experts on the immune system — immunologists — know that too much of an immune reaction could result in allergies, autoimmune disorders or chronic inflammation. On the flip side, too little of an immune reaction could result in illness or infection.
Your immune system requires a delicate balance to operate properly. When it's out of balance, your immune system itself can cause disease.
Related: New 'inverse vaccine' could wipe out autoimmune diseases, but more research is needed
Cellular balance
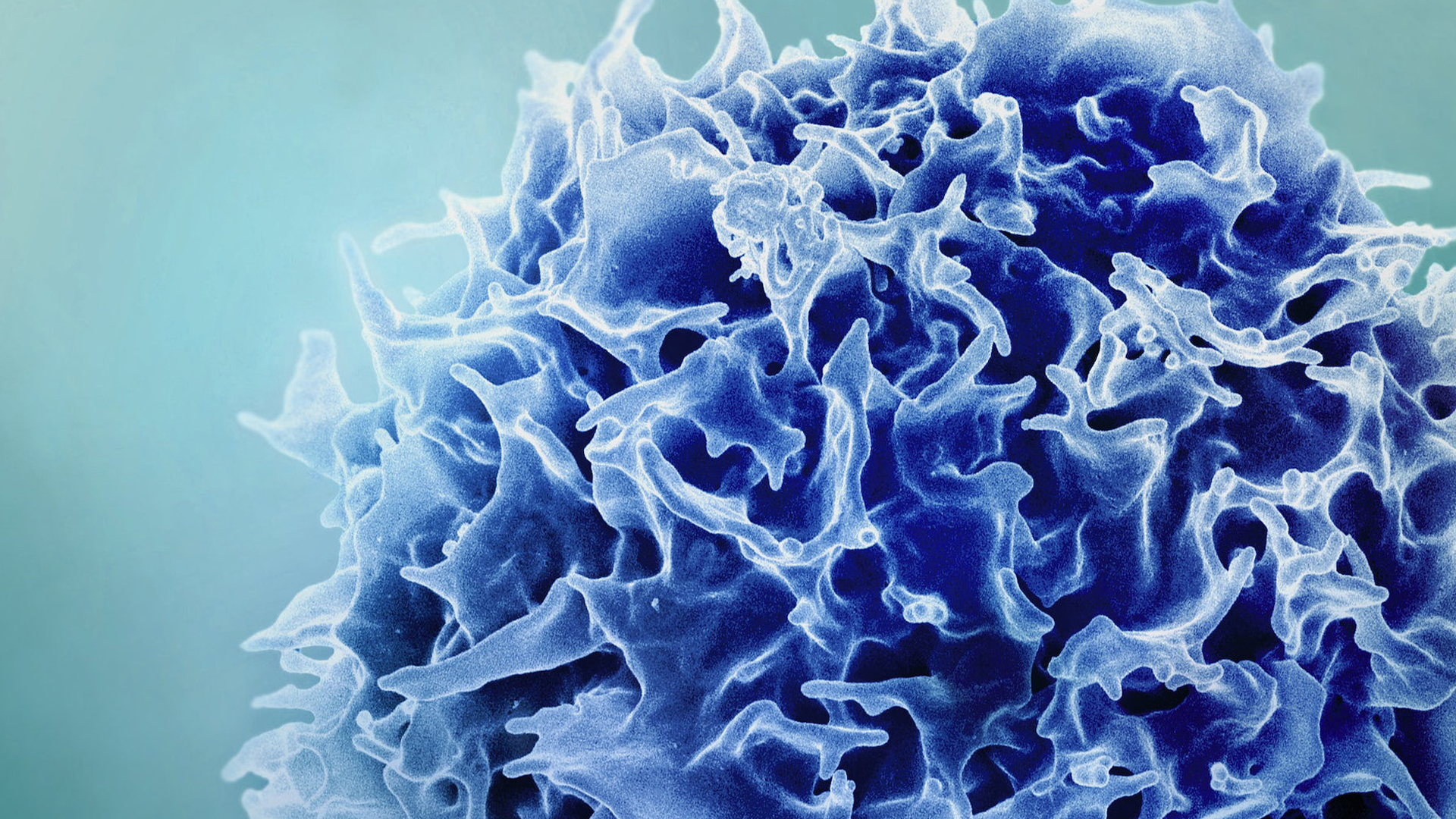
The immune system is the mobile defense system of your body. It is a complex network of cells and organs that work together to protect your body from infection and disease. Your immune cells are continually on patrol, traveling throughout your body looking for infectious invaders and damage.
New immune cells are created in your bone marrow. Certain immune cells — called B and T cells — are the special forces of the immune system, playing an important role in the elimination of infectious invaders. Because of this role, these cells undergo a rigorous boot camp during their development to ensure they will not discharge friendly fire on healthy cells in the body.
Any B cell or T cell exhibiting activity against the self — or autoreactivity — is killed during training. Millions of newly created B and T cells are killed every day because they fail this training process. If these self-reactive cells escape destruction, they could turn against the body and carry out an inappropriate autoimmune attack.
Get the world’s most fascinating discoveries delivered straight to your inbox.
My research investigates how B cells are able to slip past the checkpoints the immune system has in place to guard against autoreactivity. These tolerance checkpoints ensure that autoreactive immune cells are either purged from the body or held in permanent lockdown and unable to engage in inappropriate responses that would target healthy tissue.
More isn't necessarily better
You've likely seen advertisements for dietary supplements that promise to "boost immune function." While this may sound appealing, it is important to keep in mind that the immune system functions best when perfectly balanced.
If the immune system is like a thermostat, turning it up too high results in overactivation and uncontrolled inflammation, while turning it down too low results in a failure to respond to infection and disease.
Because sustaining immune balance is critical, tinkering with the immune system through the use of supplements is not a good idea unless you have a clinical deficiency in certain vital nutrients. For people with healthy levels of nutrients, taking supplements could lead to a false sense of security, particularly since the fine print on the back of supplements usually has this disclaimer about their listed benefits: "This statement has not been evaluated by the FDA. Not intended to diagnose, treat, cure, or prevent any disease."
Eating a well-balanced diet, exercising regularly, reducing stress and getting decent sleep, on the other hand, can help your body maintain a functioning and healthy immune system. Although these lifestyle behaviors are not foolproof, they contribute to overall good health and ultimately to a more healthy immune system.
In reality, vaccines are the only safe and effective tool beyond healthy lifestyle behaviors to support your immune system. Vaccines contain harmless forms of pathogens that help to train your immune cells to recognize and fight them. When you come into contact with the real and harmful version of the pathogen out in the wild — whether it's at a grocery store, social event or school — at a later date, these fully trained immune memory cells will immediately begin to fight and destroy the pathogen, sometimes so quickly that you don't even realize you've been infected.
In a world where people are continually bombarded by the marketing mantra that more is better, rest assured that when it comes to the immune system, maintaining perfect balance is just right.
This edited article is republished from The Conversation under a Creative Commons license. Read the original article.
Dr. Aimee Pugh Bernard has a broad background in cellular immunology and molecular biology, with specific expertise in human immunology, having attained her PhD in the developmental regulation of human B cells and the autoimmune disorder Systemic Lupus Erythematosus (SLE). As a graduate student in immunology, Aimee studied the developmental regulation of VH4.34-expressing B cells as an experimental system for the study of human B cell tolerance. Her studies revealed that mechanisms of cellular regulation during development are impaired in patients with SLE leading to a breach in self-tolerance. As a post-doctoral fellow at National Jewish Health, her research focused on the phenotypic characterization of anergic human B cells via the analysis of basal calcium levels and the ability to flux calcium after stimulation. As a post-doctoral fellow at the Barbara Davis Center, her work revealed that Nkx2.2 is required in the differentiation of pancreatic beta cells and that insulin- and ghrelin-producing cells may share a common progenitor.
Aimee is an Assistant Professor in the Department of Immunology and Microbiology at the University of Colorado Anschutz medical campus (CU AMC) and is actively involved in the CU School of Medicine (CUSOM) Trek curriculum reform, serving as the immunology content director. Aimee also teaches immunology within the medical school, graduate school, dental school, and the Child Health Advocate / Physician Assistant (CHA/PA) program on the Anschutz medical campus. At the start of the pandemic, Aimee helped to develop and run three courses for second, third and fourth year medical students that focused on the SARS-CoV-2 and COVID-19.
Aimee is dedicated to science communication and frequently delivers seminars and interactive sessions on immunology, vaccines, and science to a variety of audiences within the general public.
As a faculty mentor, she guides an amazing group of volunteer graduate students from all across campus to run a non-profit, after-school science program — Think Like a Scientist — at elementary schools throughout the Aurora and Denver communities.
In her role as the Assistant Director for the CU School of Medicine Dean's Office Human Immunology and Immunotherapy Initiative (HI3) Aimee has utilized her experience as an immunologist with expertise in human B cell development and autoimmunity, her skills as an educator and communicator of science, and her organizational and program building skills to coordinate the development of the research and clinical infrastructure necessary to create an all-inclusive, premier facility for the discovery and use of human immunotherapies for the treatment of cancer and autoimmune diseases.
 Live Science Plus
Live Science Plus






