Scientists uncover the cells that save you when water goes down the wrong pipe
In a mouse study, scientists uncovered the sensory cells that trigger coughing when you inhale water by mistake.

You take a sip of water but suddenly burst into uncontrollable coughing — your drink has "gone down the wrong pipe." It turns out that this familiar, protective response is instigated by rare, tiny cells in your airways, scientists discovered in a new study in mice.
This finding could help pave the way to new methods for treating respiratory disorders, Ziai Zhu and Xin Sun of the University of California, San Diego, wrote in a commentary of the study. The researchers behind the work suggest it could be useful for treating chronic coughs, for instance, or preventing pneumonia.
When liquid enters the windpipe that leads to the lungs, rather than being swallowed down the esophagus to the stomach, the body automatically initiates safeguarding mechanisms. These include the cough reflex, which flings the liquid out of the windpipe, and the swallowing reflex, which gulps it down into the stomach.
These reflexes help expel any inhaled fluid from the airways as soon as possible, to protect the delicate tissues in the lungs that allow us to breathe. If these protective mechanisms fail, bacteria within inhaled fluid can potentially trigger infection and inflammation in the lungs, known as pneumonia. Acid reflux triggers a similar set of reflexes when the contents of the stomach inadvertently travel back up the esophagus.
Related: New cause of asthma lung damage revealed
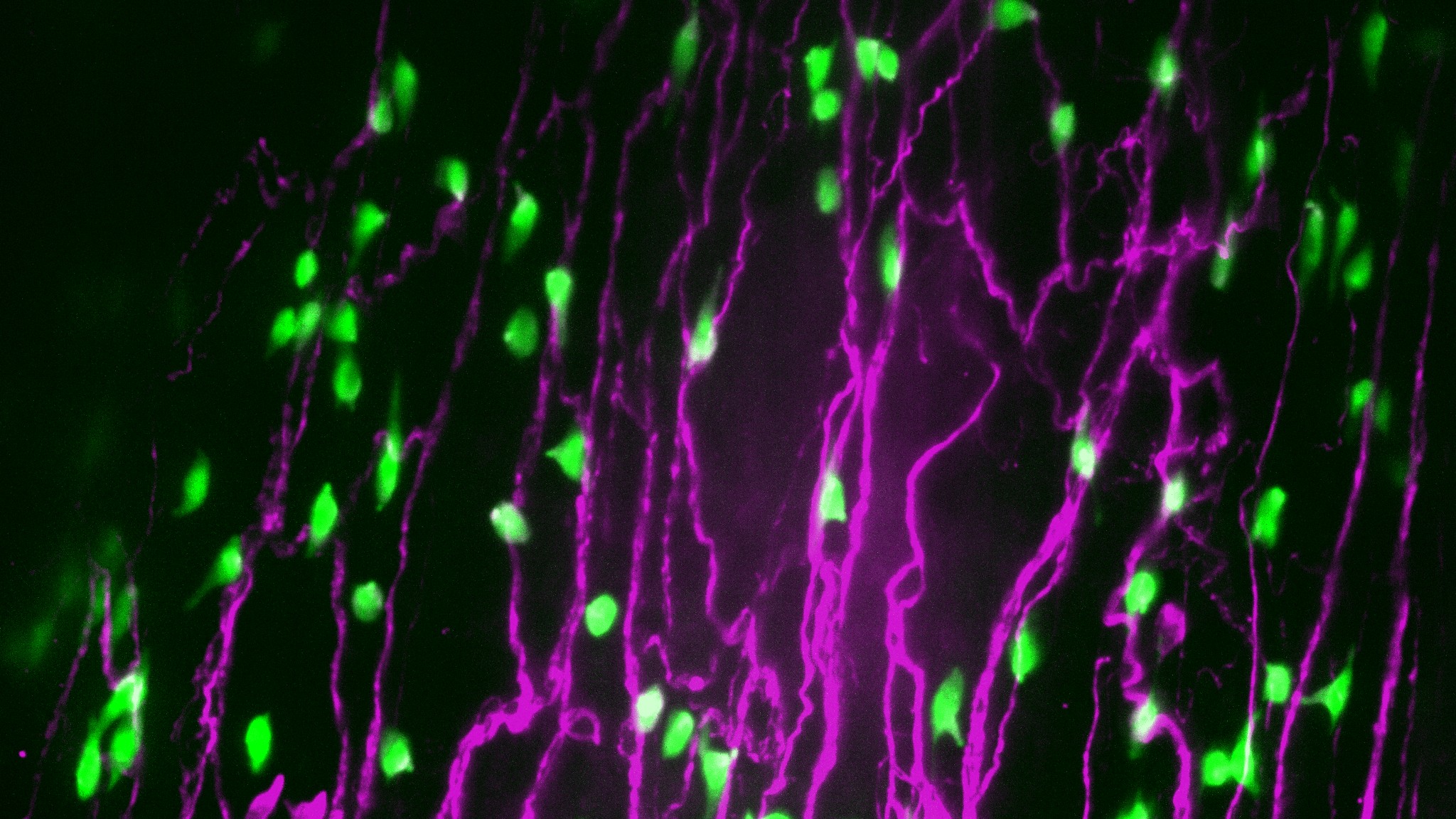
These reflexes kick in thanks to nerves in the airways that relay danger signals to the brain. But these nerves don't do it alone — now, scientists have shown that the nerves get a helping hand from special cells in the lining, or epithelium, of the voice box and windpipe. These cells are known as neuroendocrine cells, and they're considered rare because they make up less than 0.5% of the airway epithelium.
In the new mouse study, published Thursday (April 18) in the journal Science, the researchers revealed that these cells sense both water and acid in the upper airways. In response, they release a chemical called ATP that then activates nerves that shoot signals to the brain.
Get the world’s most fascinating discoveries delivered straight to your inbox.
These neuroendocrine cells were already known to be in the upper airways, because in rare cases, the cells can give rise to tumors in the voice box. However, the cells hadn't really been studied in terms of what they may be able to sense, Laura Seeholzer, co-senior study author and a postdoctoral scholar in physiology at the University of California, San Francisco, told Live Science.
"Going into this study, I generally assumed that most of this [coughing] reflex was driven by sensory neurons," Seeholzer said. "So when I found that these rare epithelial cells were also detecting these stimuli, and that they were communicating with the nervous system, it kind of clicked that 'Oh, these cells could also be really important.'"
To take another look at the cells, Seeholzer and colleagues extracted them from the lungs, voice box and upper and lower airways of mice. They examined the cells in the lab to see which of their genes were active and what stimuli caused them to release chemical signals.
They found that the neuroendocrine cells from the voice box and windpipe responded to water and acid, whereas the cells from the lungs responded to pressure, as has been shown in previous studies. When activated, these cells release ATP that, at least in mouse tissue in lab dishes, switches on sensory neurons that initiate swallowing and coughing reflexes.
In separate experiments in living mice, the team found that activating these specific neuroendocrine cells in the voicebox and windpipe made the rodents swallow and cough. On the other hand, mice genetically modified to lack these cells were less likely to swallow water that ended up in their airways than mice who had their neuroendocrine cells intact.
Since these cells seem key to triggering these protective reflexes, it's likely that their dysfunction could partly explain why some people struggle to swallow or often inhale water into their airways, Seeholzer said. Aging, for example, can make people more likely to accidentally breathe in food or water because the cough reflex can become dysfunctional.
Recent research has shown that small molecules that block ATP from plugging into a specific receptor can reduce coughing in people with chronic cough. The activation of this receptor, called P2X, had previously been found to trigger swallowing reflexes in mice, backing the idea that it's key to both reflexes.
P2X is also the receptor that neuroendocrine cells in the new study interact with. Therefore, the new findings could help uncover new treatments for chronic coughing conditions, Seeholzer said.
But, given the new research was solely in mice, the team now plans to study these neuroendocrine cells in humans. In people, they hope to address the questions of whether these cells change as we age or as a result of chronic smoking, Seeholzer said.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to community@livescience.com with the subject line "Health Desk Q," and you may see your question answered on the website!

Emily is a health news writer based in London, United Kingdom. She holds a bachelor's degree in biology from Durham University and a master's degree in clinical and therapeutic neuroscience from Oxford University. She has worked in science communication, medical writing and as a local news reporter while undertaking NCTJ journalism training with News Associates. In 2018, she was named one of MHP Communications' 30 journalists to watch under 30.
 Live Science Plus
Live Science Plus