Allergic reactions to Moderna's COVID-19 vaccine are extremely rare, report finds
There's about a 2.5 per 1 million chance of having a severe allergic reaction.
Get the world’s most fascinating discoveries delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?

Delivered Daily
Daily Newsletter
Sign up for the latest discoveries, groundbreaking research and fascinating breakthroughs that impact you and the wider world direct to your inbox.

Once a week
Life's Little Mysteries
Feed your curiosity with an exclusive mystery every week, solved with science and delivered direct to your inbox before it's seen anywhere else.

Once a week
How It Works
Sign up to our free science & technology newsletter for your weekly fix of fascinating articles, quick quizzes, amazing images, and more

Delivered daily
Space.com Newsletter
Breaking space news, the latest updates on rocket launches, skywatching events and more!

Once a month
Watch This Space
Sign up to our monthly entertainment newsletter to keep up with all our coverage of the latest sci-fi and space movies, tv shows, games and books.

Once a week
Night Sky This Week
Discover this week's must-see night sky events, moon phases, and stunning astrophotos. Sign up for our skywatching newsletter and explore the universe with us!
Join the club
Get full access to premium articles, exclusive features and a growing list of member rewards.
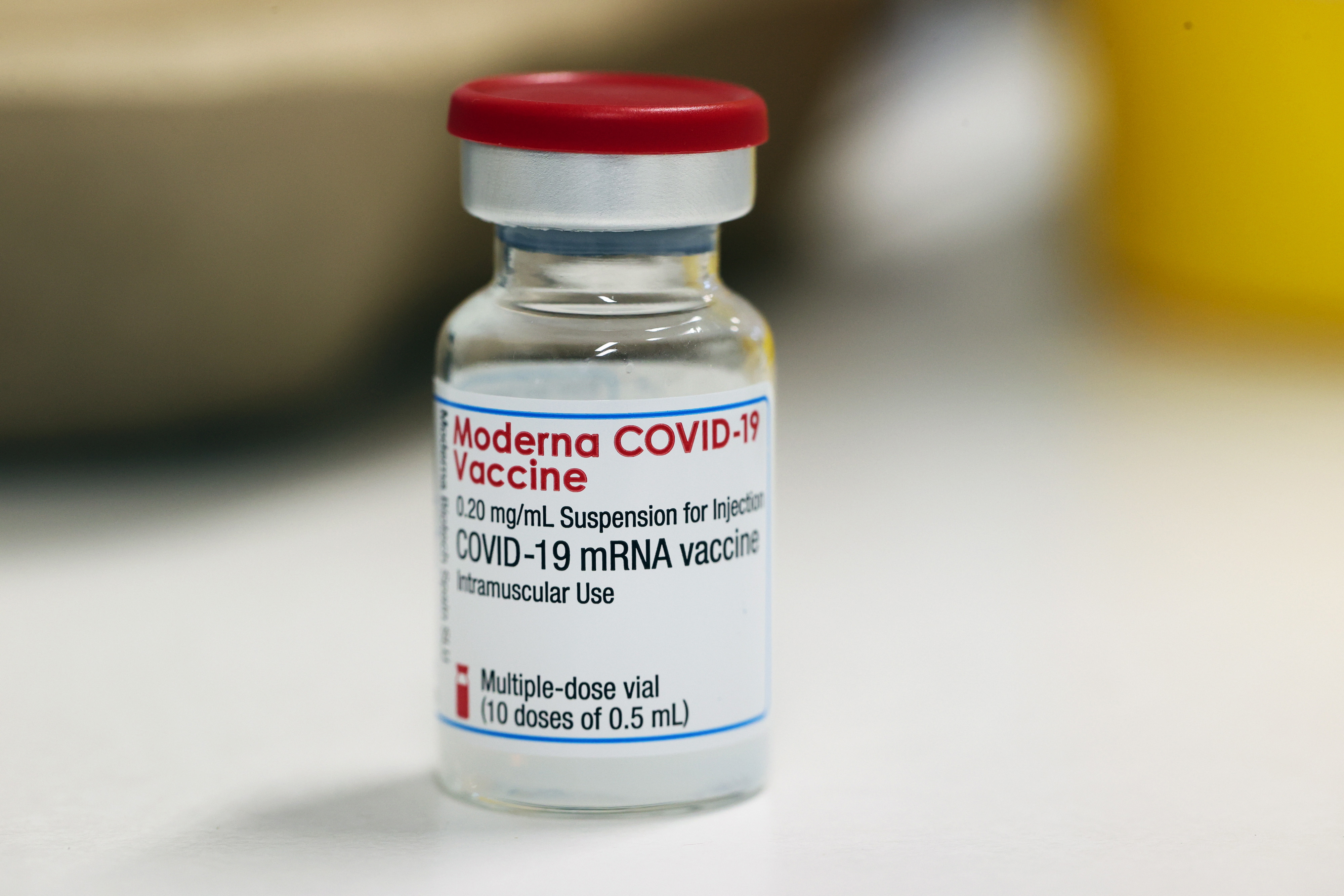
Moderna's COVID-19 vaccine rarely causes severe allergic reactions, according to new data released by the Centers for Disease Control and Prevention (CDC).
Between Dec. 21 and Jan. 10, more than 4.04 million people were given Moderna's COVID-19 vaccine, but only 10 developed a serious, potentially life-threatening allergic reaction called anaphylaxis. That works out to be around 2.5 cases of anaphylaxis per 1 million people vaccinated, according to the CDC's Morbidity and Mortality Weekly Report.
It's not yet clear what's causing the severe allergies, but nine out of 10 of these cases occurred among patients with previously known allergies (five previously had anaphylaxis). Most had
allergies to various medicines such as penicillin, but one had environmental and food allergies and another didn't have any prior known allergies, according to the report.
Related: 14 coronavirus myths busted by science
Nine out of 10 of the patients developed symptoms — such as vomiting, nausea, wheezing, tongue swelling and rash — within 13 minutes of getting the vaccine and one developed symptoms within 45 minutes.
All 10 patients were treated with epinephrine — a hormone also known as adrenaline that is the key ingredient in EpiPens and similar autoinjectors; four were treated in an emergency department and six were hospitalized, with four requiring intubation. But all 10 patients recovered, according to the report.
Get the world’s most fascinating discoveries delivered straight to your inbox.
"Based on this early monitoring, anaphylaxis after receipt of Moderna COVID-19 vaccine appears to be a rare event," the authors wrote in the report. But because there's not yet widespread data on COVID-19 vaccines, it's difficult to compare the risk of anaphylaxis with non-COVID-19 vaccines, they wrote. In a previous Morbidity and Mortality Weekly Report, published on Jan. 15, researchers estimated that the Pfizer-BioNTech vaccine causes anaphylaxis in about 11.1 cases per million doses (0.001% chance); that estimate was based on early data.
Still, both the anaphylaxis associated with both Pfizer's and Moderna's COVID-19 vaccines seems to be above the average number of anaphylaxis cases found for previous vaccines. In 2015, researchers calculated that the chance of developing a severe allergic reaction to a vaccine is about 1.31 in 1 million, according to a 2015 study published in the Journal of Allergy Clinical Immunology. "True allergic reactions to vaccines are very rare," Dr. Purvi Parikh, allergist and immunologist at NYU Langone Health, previously told Live Science. "Statistically, you're more likely to be hit by lightning than have a true anaphylactic reaction to a vaccine." Though the cases are extremely rare — and should not dissuade people from getting the vaccine — experts are working on identifying what could be causing the allergies.
People who have had an allergic reaction to the first dose of the vaccine should not receive the second dose, the authors wrote. Vaccine centers should have all the necessary supplies and trained staff to treat anaphylaxis, they wrote. The CDC also recommends that people who receive COVID-19 vaccines should also be monitored for about 15 minutes, or 30 minutes if they have a history of allergies or anaphylaxis.
Originally published on Live Science.

Yasemin is a staff writer at Live Science, covering health, neuroscience and biology. Her work has appeared in Scientific American, Science and the San Jose Mercury News. She has a bachelor's degree in biomedical engineering from the University of Connecticut and a graduate certificate in science communication from the University of California, Santa Cruz.
 Live Science Plus
Live Science Plus










