'Stiff Person Syndrome' Treated by Stem Cell Transplant
People with a rare disease called stiff person syndrome, or SPS, might benefit from a type of stem cell transplant that has been used to treat patients with leukemia and multiple sclerosis, researchers say.
SPS is a neurological condition that causes people to suffer from periodic muscle stiffness and spasms that make everyday activities like walking or driving a car extremely difficult. Symptoms are often triggered by stress or environmental factors such as loud noises or cold temperatures.
People with SPS are usually treated with medications that aim to control their spasms or, in more severe cases, seizure medications. The new study shows that patients who aren't helped by the medications might benefit from a treatment called autologous hematopoietic stem cell transplantation, or auto-HSCT, which involves removing and storing a patient's own bone marrow cells, and then reinjecting them, according to the researchers at the Ottawa Hospital Research Institute in Ottawa. [Inside Life Science: Once Upon a Stem Cell]
Such stem cell transplants have been used along with chemotherapy to treat patients with multiple sclerosis, according to the Ottawa-based doctors. The procedure is also used with chemotherapy to treat patients with leukemia, said Dr. Ruthee-Lu Bayer, director of stem cell transplantation at North Shore-LIJ Cancer Institute in Lake Success, New York.
"When we give a person an autologous stem cell transplant, it's because we want to be able to give that person a higher dose of chemotherapy to kill off more tumor cells," Bayer told Live Science. "This higher dose of chemo kills off the tumor cells, but also shuts off the bone marrow factory where blood cells are made." The transplant replaces those lost bone marrow cells.
In the case of patients with SPS, the role of chemotherapy is to kill off diseased immune cells, not tumor cells, but the effect is the same: The bad cells die, but so do some good ones. [7 Side Effects of Cancer Treatment, and How to Cope with Them]
The stem cell transplant starts before chemotherapy treatment begins, with the doctors removing bone marrow cells, including stem cells, from the patient. The cells are then stored and reintroduced into the patient's body once chemotherapy is over.
Get the world’s most fascinating discoveries delivered straight to your inbox.
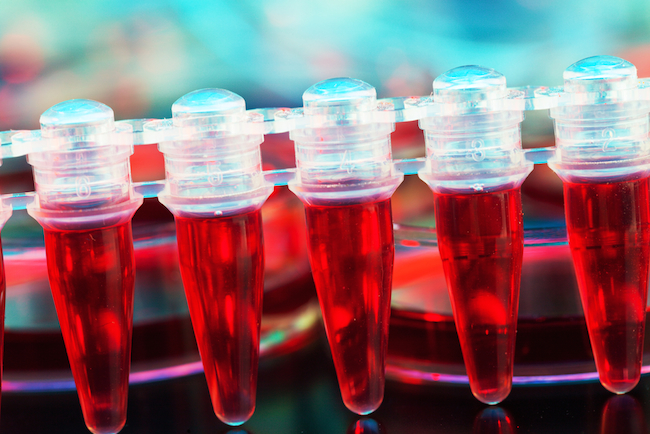
Collecting blood
Collecting stem cells typically takes a few days, Bayer said. To get at the particular cells that are needed — hematopoietic stem cells — doctors give patients an injection of what's known as a growth factor, which wrests the cells out of the bone marrow and into the bloodstream, said Dr. Christopher Bredeson, a senior scientist at the Ottawa Hospital Research Institute and co-author of the new case report.
Once the stem cells are circulating in the blood, the patient is hooked up to a device called an apheresis machine. Blood is taken out of the patient's body and spun around to separate it into its components, and the stem cells are then collected from the machine while the rest of the blood is returned to the patient.
To treat patients with SPS, Bredeson and his colleagues included an extra step in the blood collection process. They filtered the blood to make sure that no diseased immune cells were included with the healthy stem cells collected from the patient.
"In the blood that we collect are the stem cells but also mature immune system cells, or T-cells, that we don't want," because these are the cells that drive SPS in the first place, Bredeson told Live Science.
To do this separation, the doctors mixed an antibody into the collected blood that would attach itself only to stem cells, not mature T-cells. The antibody contained a tiny piece of iron. The doctors then poured the blood through a funnel-like device embedded with magnets, and the iron-laden stem cells stuck to the magnets while the rest of the blood poured through the funnel.
In this way, the doctors were able to transplant only the cells they wanted into the patient after chemotherapy.
New blood
For people with SPS, as well as people with multiple sclerosis and other diseases, this lengthy procedure resets the immune system.
"It's just like you're a baby again," Bredeson said. The stem cells make copies of themselves, repopulating the bone marrow with healthy cells, "and start everything over again from scratch. Your whole immune system grows up again, just like when you were made the first time," he added.
Therefore, people who receive this treatment need to be revaccinated, and also need to take certain medications to prevent bacterial and viral infections.
Chemotherapy and auto-HSCT have been used by the Ottawa doctors, as well as doctors elsewhere, to keep the symptoms of multiple sclerosis at bay for up to five years, Bredeson said. And in the case of the two patients with SPS who received the treatments, symptoms have abated for up to 4.5 years, according to the recent case report.
However, more patients need to be treated using auto-HSCT before the doctors can determine how effective this treatment option is, the researchers said.
The case report was published Monday (Aug. 25) in the Journal of the American Medical Association.
Follow Elizabeth Palermo @techEpalermo. Follow Live Science @livescience, Facebook & Google+. Original article on Live Science.
 Live Science Plus
Live Science Plus





