Implantable Lazy Susans Could Deliver Drug Cocktails
Many drugs would work better, and so could be used in smaller amounts, if they could be delivered to just the right place at exactly the right time.
Remote-controlled, drug-dispensing "lazy Susans" may be the answer. These devices can dole out a smorgasbord of solid, liquid, or gel-based drugs.
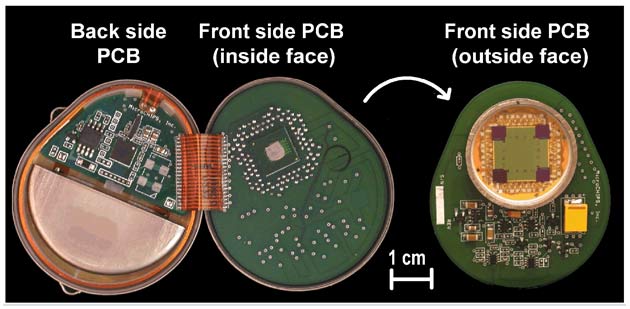
The current model of this device is implanted just under the skin. It is just over a half-inch (15 millimeters) square and contains 100 little reservoirs, each of which contains a tiny amount of a drug. Sealing each reservoir is a membrane, a metal sandwich of titanium inside with outer layers of platinum. This membrane is just 3,800 angstroms thick, about a third of one percent as thick as a human hair.
Startup company MicroCHIPS, of Bedford, Massachusetts, is developing the device. Each reservoir holds 300 nanoliters of a drug. That's 300 billionths of a liter or about 0.000011 of a fluid ounce. Future models, however, could have any number of reservoirs with different capacities, says MicroCHIPS president John Santini, who over the last decade developed the technology with a team of Massachusetts Institute of Technology scientists.
"We're able to use wireless technology to control it, along with microprocessors, and batteries for power. We can actively turn it on and off to control how much drug comes out and when," Santini says. "When we want to release the drug, we send a small electric current through a membrane that is covering the opening of this reservoir."
When the microchip in the device receives a transmission from outside the body, it directs the 3-to-4-volt, 1-amp electric current for 10 to 20 microseconds, about a two thousandth of a blink of the eye, toward a specific reservoir, eroding the membrane that covers it and releasing the drug inside. While the thing does not actually rotate, it can open any combination of reservoirs, releasing drug cocktails or varying a drug's dosage.
The company is developing a similar technology, Santini says, for implantable sensors. Devices that monitor changes in body chemistry find humans to be harsh environments in which to survive and can quickly lose their effectiveness. This new technology could be used to build devices that contain hundreds of monitors. As each wears out, the device could open another membrane, exposing another sensor. As with drugs, a single package could carry many types of monitors.
Get the world’s most fascinating discoveries delivered straight to your inbox.
It is even possible, Santini says, that a single device could house sensors and drugs—for example, blood-sugar monitors and insulin for diabetics.
The company tested implanted drug-dispensing devices in six beagles, drug-reservoir dogs, if you will, for six months. Human trials are at least a few years away.
 Live Science Plus
Live Science Plus





