Epidurals: How They've Changed, and How They Work

The modern epidural — a powerful combination of painkillers used to help women endure labor — is nothing like the painkillers of generations past.
These days, about two-thirds of women in the U.S. have epidurals during labor, said Dr. Aaron Caughey, professor and chair of the Department of Obstetrics and Gynecology at Oregon Health and Science University.
The procedure has undergone major changes since the earliest days of using drugs to help women in labor manage their pain. [8 Odd Changes That Happen During Pregnancy]
In the most recent change, made in the early 2000s, anesthesiologists greatly lowered the dose of the drugs used in an epidural, and they gave women a button they could press if they needed more pain relief.
"We're using less drug, and more of it is patient-controlled," said Dr. Stephen Halpern, an obstetric anesthesiologist at Sunnybrook Health Sciences Centre in Toronto. "Instead of me deciding on the dose, we give the patient a button to push, and if she needs more, she pushes it."
But women were not always given such control.
In 1900, at least one U.S. doctor used cocaine as an anesthetic during labor or, as he put it, a "cocainization of the spinal cord," according to a 2010 study published in the journal Local and Regional Anesthesia.
Get the world’s most fascinating discoveries delivered straight to your inbox.
In the decades that followed, doctors began using flexible tubes called catheters to deliver the medicine. The end of the tube was inserted under the skin and was used to deliver the drug whenever it was needed, so doctors didn't have to continuously jab laboring women with needles. But these epidurals were still a long way off from those of today.
In the 1970s, anesthesiologists would insert a catheter tube and use it manually to deliver a dose of pain medicine every 2 hours, Halpern said.
This wasn't ideal, because if a woman was in labor for a long time — say 20 hours — she would need 10 doses. That many doses could make her lose all sensation below her waist and, in turn, make it difficult for her to push or feel feedback from the labor, experts told Live Science.
In the mid-1980s to early 1990s, doctors began delivering epidurals using a continuous infusion, meaning that the catheter would continuously deliver the drugs until the woman delivered the baby. But still, some women complained of "heavy legs," indicating that their doses were too high, Halpern said.
In today's epidurals, women are given about a quarter of the dose of drugs that they were given back then, Halpern said.
How an epidural works
Epidurals may contain anesthetic agents, such as bupivacaine or ropivacaine, that numb the area.They may also be given narcotics, including fentanyl, that diminish — but do not eliminate — the pain. Or, they may get a mixture of anesthetics and narcotics, Halpern said.
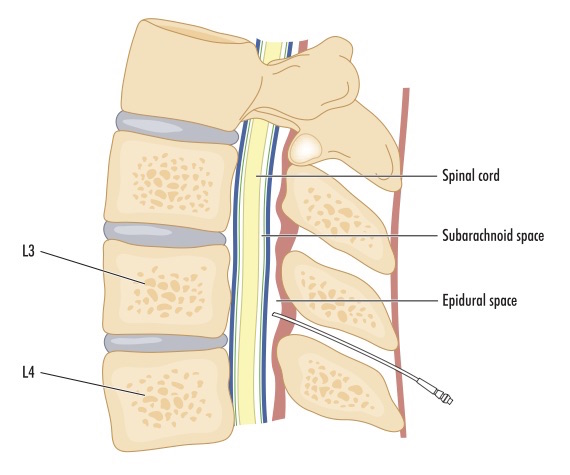
The modern epidural is a continuous infusion of drugs, delivered through a catheter into an area called the epidural space, in the lower back, Caughey said.
The epidural is usually administered during the first stage of labor, when the woman's cervix has dilated to about 4 inches (10 centimeters), Caughey said. It takes about 15 minutes for the drugs to start working; and although the drug infusion may be turned off at some point, the catheter is kept in until after the delivery, so the infusion can be turned back on if the woman experiences more pain. For example, some women may need stitches or other treatments to repair lacerations that occurred during the birth, he said.
If the woman needs a Cesarean section, the doctors can use the epidural catheter during the procedure, Caughey said.
Most epidurals cost between $700 and $1,200, which includes the fee for the anesthesiologist and the hospital equipment, Caughey said.
The pros
The benefits of epidurals include:
- Pain relief that allows women in labor to remain awake and alert, Halpern said. (Other pain management options for women in labor include intravenous narcotics or a shot of morphine, which do not allow the women to remain awake or alert, he said.)
- If women have complications, such as high blood pressure (preeclampsia), the epidural can help to lower her blood pressure, Halpern said. Or, if she is having twins, the epidural can help manage the pain during a particularly long labor, he said.
- Epidurals do not have any effect on fetal oxygenation or the baby's 5-minute Apgar scores (a test that measures the newborn's physical condition), nor do they increase the rate of women who need cesarean sections, according to a 2002 review in the American Journal of Obstetrics and Gynecology that Halpern co-authored.
The cons
Epidurals have several drawbacks, including the following:
- For reasons that aren't yet clear, epidurals are associated with an increase in the woman's oral and vaginal temperature. If the woman's temperature increases, doctors may treat her with antibiotics, just in case the high temperature is due to bacterial infection, Caughey said. [7 Baby Myths Debunked]
- In general, epidurals lengthen labor. In a study of more than 42,000 women in California who delivered vaginally between 1976 and 2008, women who received epidurals took more time to "push out" the baby, according to a 2014 study in the journal Obstetrics & Gynecology that Caughey co-authored. First-time mothers who received an epidural took about 5 and a half hours to deliver their baby, compared with about 3 and a half hours for women who didn't receive an epidural, they found.
- Epidurals are linked to drops in the woman's blood pressure, which can affect the baby's heart rate, according to the Mayo Clinic.
- In 2 percent of cases, women develop severe headaches that can last for days. This happens when the doctor inserting the epidural punctures the dura, a membrane or a cover holding the cerebrospinal fluid that surrounds the brain and spinal cord. If the needle punctures the dura, some of the fluid can leak out, leading to a headache, Halpern said.
- Epidural anesthesia can impair a woman's ability to empty the bladder, so many women need to temporarily use a catheter to urinate, the Mayo Clinic reported.
- The epidural makes some women feel itchy, according to the Mayo Clinic.
Original article on Live Science.

Laura is the managing editor at Live Science. She also runs the archaeology section and the Life's Little Mysteries series. Her work has appeared in The New York Times, Scholastic, Popular Science and Spectrum, a site on autism research. She has won multiple awards from the Society of Professional Journalists and the Washington Newspaper Publishers Association for her reporting at a weekly newspaper near Seattle. Laura holds a bachelor's degree in English literature and psychology from Washington University in St. Louis and a master's degree in science writing from NYU.