Severe Burns May Let 'Bad Bacteria' Take Over the Gut
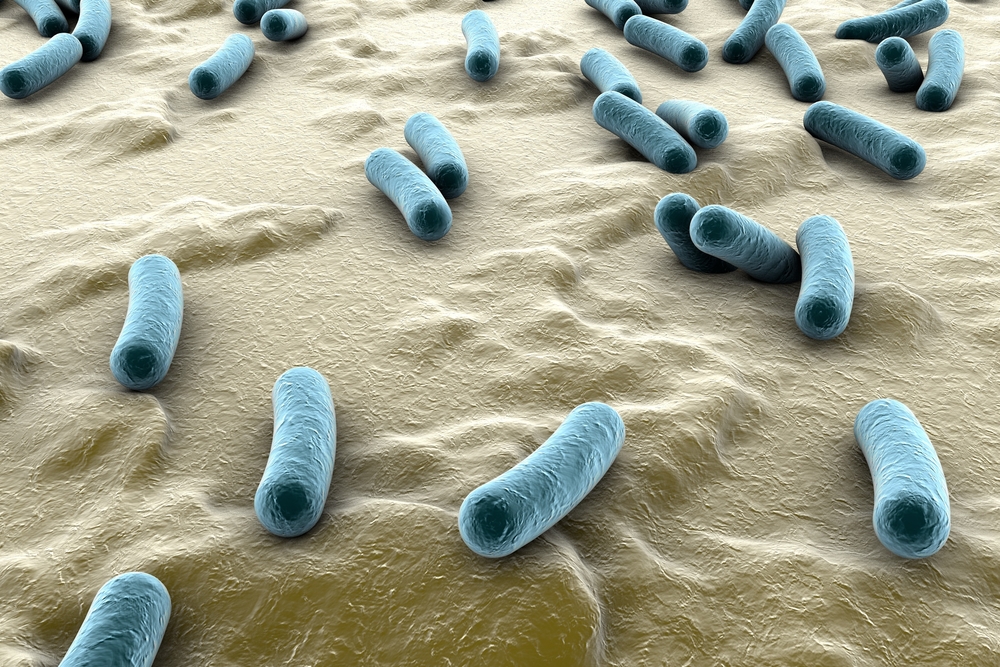
People who have gotten severe burns are known to be at risk for a host of complications, but there may be other consequences lurking deeper within the body: A new study finds that a burn may change the community of bacteria within a person's gut, and possibly lead to an increased risk of infection.
In the study, researchers analyzed fecal bacteria from four patients with severe burns over at least 30 percent of their body, and compared these bacteria with fecal bacteria of people with minor burns. They found that the severely burned patients had higher levels of a potentially dangerous group of bacteria called Enterobacteriaceae, which includes E. coli and Salmonella.
In fact, Enterobacteriaceae made up 31.9 percent of the gut bacteria in the people with severe burns, compared with just 0.5 percent in those with minor burns, according to the study, published today (July 8) in the journal PLOS ONE.
The results are preliminary, but they indicate that the bacteria in the gastrointestinal system, called the microbiome, may offer a path for doctors to help severely burned patients, said Mashkoor Choudhry, senior author of the study and a professor of microbiology at Loyola University in Chicago. [5 Ways Gut Bacteria Affect Your Health]
"What it shows [is] that the biome can be used as a target to medically intervene ... to see if that manipulation helps the burn victim," Choudhry told Live Science.
The researchers also used mice to replicate the findings, and found that mice with significant burns had higher levels of Enterobacteriaceae one to three days after they were burned, according to the study.
This increase in "bad bacteria" may explain why burn patients are at increased risk for sepsis, a dangerous inflammatory response that can lead to organ failure, Choudhry said. It's possible that the severe burns compromise the defense mechanism in the gut, thus allowing the harmful bacteria to leave the gut and trigger inflammation in the body, Choudhry noted.
Get the world’s most fascinating discoveries delivered straight to your inbox.
Choudhry and his colleagues speculated that probiotics — "good" bacteria aimed at improving digestive health— may help treat people who have higher levels of harmful bacteria and decrease their risk of sepsis or bacterial infections. However, they did not test whether probiotics were beneficial for patients during this study.
Dr. Nikolaos Pyrsopoulos, director of gastroenterology and hepatology at New Jersey Medical School and an associate professor at Rutgers University, said the findings are preliminary but are part of a larger effort in the medical community to understand how the human microbiome can affect many human diseases.
"I believe we are in the dawn of a new era" of investigations into how the human microbiome can affect people's health, said Pyrsopoulos, who was not involved in the new study. "Now, we know we have more than 3 pounds of bacteria in our body, [and] how important it is to look at [the] composition of this bacteria."
When a person undergoes severe trauma, such as a large burn, the blood flow to the gut can diminish, leading to the death of the cells that collect nutrients in the intestines, Pyrsopoulos said. As a result, he added, the wall of the intestines can become more permeable, allowing bacteria to travel to other parts of the body and cause infection and inflammation.
For example, Enterobacteriaceae may get into a person's lymph nodes, and spread from there, potentially causing sepsis or a dangerous infection, he said.
Pyrsopoulos said that, in the future, he expects that trauma doctors will recommend probiotics or other treatments aimed at balancing gut bacteria and keeping harmful bacteria from overcolonizing the gut.
Follow Live Science @livescience, Facebook & Google+. Originally published on Live Science.