Nitric Oxide Doesn't Help Sickle-Cell Disease Patients
Get the world’s most fascinating discoveries delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?

Delivered Daily
Daily Newsletter
Sign up for the latest discoveries, groundbreaking research and fascinating breakthroughs that impact you and the wider world direct to your inbox.

Once a week
Life's Little Mysteries
Feed your curiosity with an exclusive mystery every week, solved with science and delivered direct to your inbox before it's seen anywhere else.

Once a week
How It Works
Sign up to our free science & technology newsletter for your weekly fix of fascinating articles, quick quizzes, amazing images, and more

Delivered daily
Space.com Newsletter
Breaking space news, the latest updates on rocket launches, skywatching events and more!

Once a month
Watch This Space
Sign up to our monthly entertainment newsletter to keep up with all our coverage of the latest sci-fi and space movies, tv shows, games and books.

Once a week
Night Sky This Week
Discover this week's must-see night sky events, moon phases, and stunning astrophotos. Sign up for our skywatching newsletter and explore the universe with us!
Join the club
Get full access to premium articles, exclusive features and a growing list of member rewards.
Nitric oxide does not relieve pain in patients with sickle-cell disease, a new study finds.
Patients in the study treated with nitric oxide for pain fared no better in terms of the length of their pain episodes than those who inhaled a placebo, the study found.
Inhaling the gas also did not shorten patients' hospital stays, or the amount of pain medication they took.
Patients with sickle-cell disease suffer pain when misshapen blood cells clog their blood vessels. Nitric oxide relaxes blood vessels and improves blood flow. Previously, two smaller studies suggested breathing nitric oxide reduced pain and medication use in sickle-cell patients.
But the new findings take nitric oxide off the table as a therapeutic drug for sickle-cell disease, said study researcher Dr. Gregory Kato, head of National Heart, Lung and Blood Institute's Sickle Cell Vascular Disease Section. Developing new treatments is critical because only one drug, called hydroxyurea, has been approved by the U.S. Food and Drug Administration to mollify patients' pain, and not all patients respond to it.
The researchers are not discouraged by their results.
"All of my collaborators on this study are not disheartened, but are dedicated to advancing the treatment of sickle-cell disease and will go on to test additional treatments in the future," Kato said.
Get the world’s most fascinating discoveries delivered straight to your inbox.
The new study will be published tomorrow (March 2) in the Journal of the American Medical Association.
Sickle-cell disease and pain crises
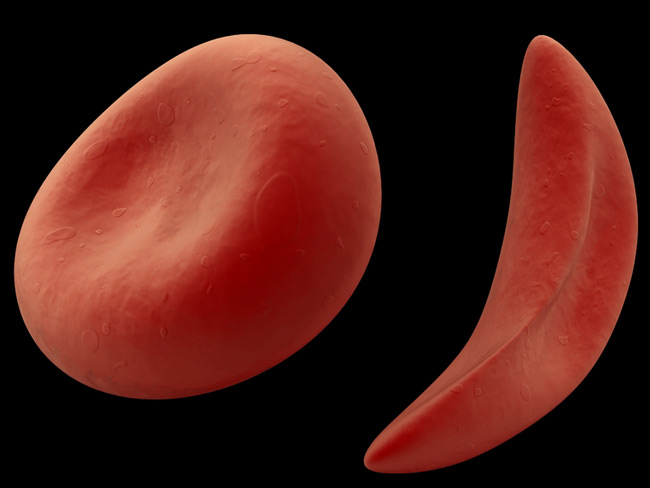
Sickle-cell disease is a hereditary condition in which the shape of red blood cells become distorted— they are sometimes C-shaped instead of their normal doughnut shape. The misshapen cells can block blood vessels, leading to pain, organ and nerve damage and stroke. Episodes of intense pain, which doctors call pain crises, are common— an average patient has two per year, though the number can vary widely — and require hospitalization, the researchers said.
People with sickle-cell disease may have sickle-cell anemia, the most severe form of the disease, or sickle-cell trait, a less-severe form. In the United States, 70,000 to 100,000 African-Americans are estimated to have sickle-cell anemia, according to the Centers for Disease Control and Prevention.
Kato and his colleagues examined the effectiveness of nitric oxide in reducing pain in 150 patients with sickle-cell disease between October 2004 and December 2008. Upon hospitalization, patients were randomly assigned to receive nitric oxide or a nitrogen gas placebo. Patients inhaled the gas for up to 72 hours.
The nitric oxide treatment was safe, but did not treat the pain. The pain crises of patients given nitric oxide lasted 73 hours, whereas they lasted 65 1/2 hours in those who received the placebo. Patients were considered recovered once they had not taken pain medication for 5 hours, rated their pain level as 6 or lower on a scale of 0 to 10, and decided, along with their family and physician, that their pain could be managed at home.
The researchers also found that patients who received nitric oxide were hospitalized for an average of 4.1 days, while those who received the placebo were hospitalized for 3.1 days.
Why doesn't it work?
The researchers don't know why nitric oxide treatment showed benefits in earlier studies, but not in the new study. It's possible that the previous findings in smaller studies were due to chance, Kato said.
The new study provides a framework for how new drugs should be tested for the treatment of sickle-cell disease, Kato said.
"It's time for us to look for additional new treatments that are being developed in the drug pipeline," Kato said.
Pass it on: Inhaling nitric oxide does not appear to provide a therapeutic benefit for patients with sickle-cell disease.
Follow MyHealthNewsDaily staff writer Rachael Rettner on Twitter @RachaelRettner.
This story was provided by MyHealthNewsDaily, a sister site to LiveScience.

Rachael is a Live Science contributor, and was a former channel editor and senior writer for Live Science between 2010 and 2022. She has a master's degree in journalism from New York University's Science, Health and Environmental Reporting Program. She also holds a B.S. in molecular biology and an M.S. in biology from the University of California, San Diego. Her work has appeared in Scienceline, The Washington Post and Scientific American.
 Live Science Plus
Live Science Plus










