Ulcerative colitis: symptoms, causes and treatment
Everything you need to know about ulcerative colitis
Get the world’s most fascinating discoveries delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?

Delivered Daily
Daily Newsletter
Sign up for the latest discoveries, groundbreaking research and fascinating breakthroughs that impact you and the wider world direct to your inbox.

Once a week
Life's Little Mysteries
Feed your curiosity with an exclusive mystery every week, solved with science and delivered direct to your inbox before it's seen anywhere else.

Once a week
How It Works
Sign up to our free science & technology newsletter for your weekly fix of fascinating articles, quick quizzes, amazing images, and more

Delivered daily
Space.com Newsletter
Breaking space news, the latest updates on rocket launches, skywatching events and more!

Once a month
Watch This Space
Sign up to our monthly entertainment newsletter to keep up with all our coverage of the latest sci-fi and space movies, tv shows, games and books.

Once a week
Night Sky This Week
Discover this week's must-see night sky events, moon phases, and stunning astrophotos. Sign up for our skywatching newsletter and explore the universe with us!
Join the club
Get full access to premium articles, exclusive features and a growing list of member rewards.
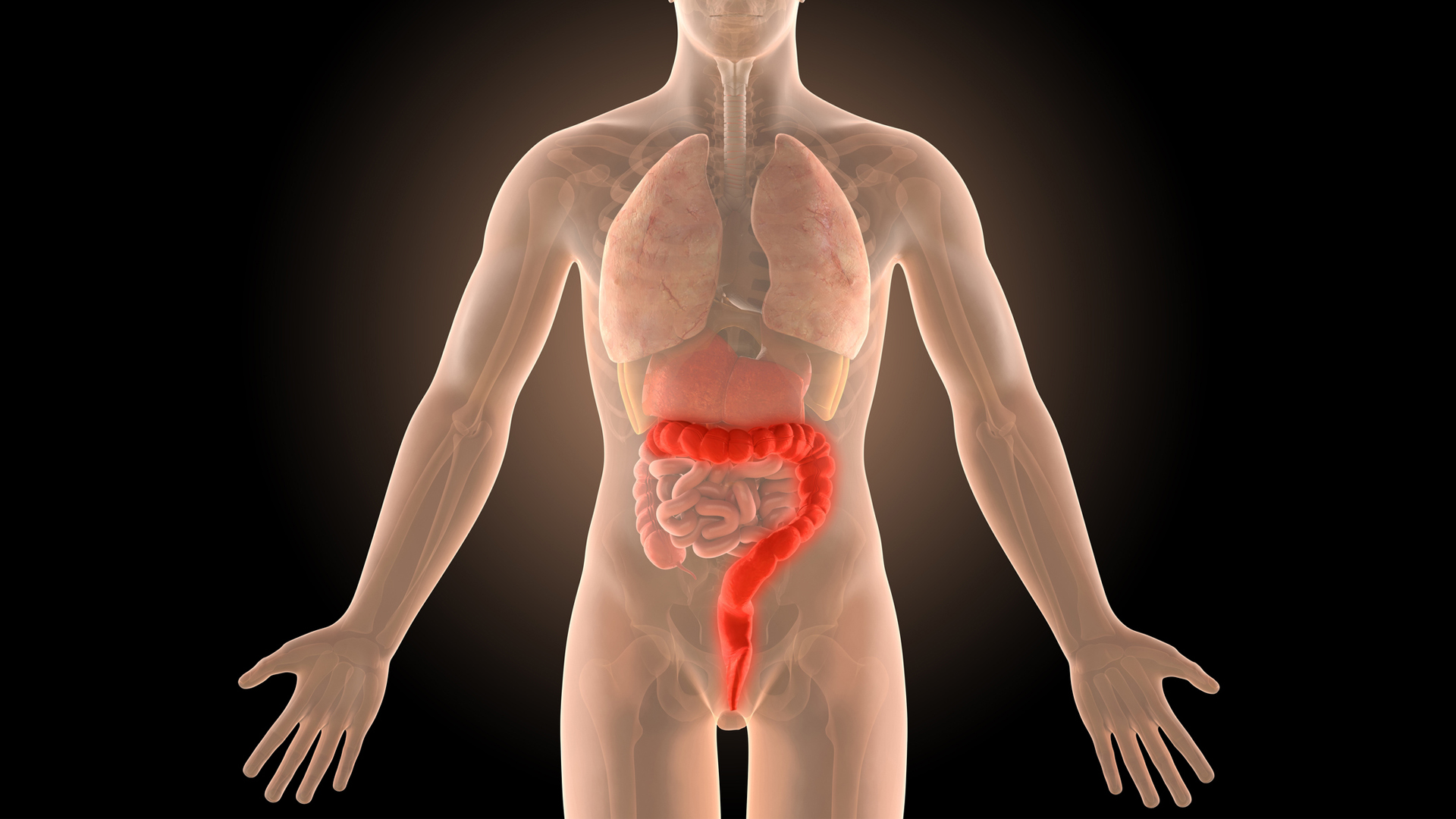
Ulcerative colitis is a complex digestive disease that presents in a variety of different ways, making it difficult to diagnose. Although we do not know what causes ulcerative colitis, it is thought to be an autoimmune condition in which the immune system attacks the gut wall, as it perceives the bacteria living there as threats that need to be eliminated.
Symptoms range from mild to severe, with complications sometimes becoming life threatening. Here, we’ll address possible causes of ulcerative colitis, as well as symptoms, diagnosis and potential tools for the management of symptoms. In particular, we will investigate how diet can impact symptoms of ulcerative colitis and whether there are foods people with the condition should be avoiding. LiveScience also spoke to medical experts to see how best to manage the condition.
What is ulcerative colitis?
Ulcerative colitis is a type of irritable bowel disease that causes irritation and ulcers in the digestive tract. There are several types of ulcerative colitis, according to the Mayo Clinic:
- Ulcerative proctitis: This type of colitis is confined to the area closest to the rectum. Rectal bleeding may be the only sign of the disease.
- Proctosigmoiditis: Inflammation spreads from the rectum and the lower end of the colon (sigmoid colon). Symptoms include abdominal cramping, bloody diarrhea, and an inability to empty the bowels although you have the urge to do so (tenesmus).
- Left-sided colitis: Inflammation spreads from the rectum up through both the sigmoid and descending colon. Symptoms are the same as proctosigmoiditis with pain further up the left side.
- Pancolitis: This usually involves the entire colon. Bloody diarrhea will be severe, there is also likely to be abdominal cramping, fatigue, and significant weight loss with this type.
Dr Ross Perry, GP and medical director of Cosmedics, tells LiveScience: “Ulcerative Colitis is a condition where the colon and rectum become inflamed,” he says. “The colon is the large intestine [bowel] and the rectum is at the end of the bowel where our stools are stored. Small ulcers can develop on the colon’s lining which can be extremely unpleasant as they can bleed and produce pus alongside a number of symptoms.”
Ulcerative colitis can reach a severity where a hole develops in the bowel lining, causing leakage into the abdominal cavity. This can be life threatening and cause sepsis, so it is important to get a correct diagnosis and the right support for this condition. It may also increase your risk of developing colon cancer, according to the journal of Surgical Oncology Clinics of North America.
Dr Deborah Lee, of Dr Fox Online Pharmacy, also explains: “It starts in the rectum and spreads proximally within the colon – the large bowel,” she says. “Bowel wall inflammation makes the colonic epithelium (the cells lining the bowel wall) thin and friable. Superficial erosions develop with frequent bleeding.”

Ulcerative colitis: Causes and symptoms
Ulcerative colitis is symptomatically similar to Crohn's disease and irritable bowel syndrome, so it can be difficult to diagnose. Dr Perry tells us that the cause of colitis is unknown, but symptoms are fairly consistent.
Get the world’s most fascinating discoveries delivered straight to your inbox.
“Symptoms can include frequent diarrhea and tummy pain, your stools may also contain blood,” he says. “Weight loss, tiredness and lack of appetite are also linked. Ulcerative colitis is thought to be an autoimmune condition in that the immune system mistakes harmless bacteria inside the colon as a threat and attacks the tissues of the colon, resulting in the area becoming inflamed and ulcers developing. No one really understands why this affects some people and not others but there is a suggestion of genetics and environmental factors.”
Common symptoms include:
- Bloody diarrhea
- Mucus or pus in stool
- Fatigue
- Abdominal pain
- Weight loss
- Skin or eye irritation
- Arthritis
- Mouth ulcers
Dr Lee explains that ulcerative colitis is a disease that is generally diagnosed young: “Most commonly ulcerative colitis is diagnosed in patients between the ages of 10 and 20. There is then a peak in diagnoses between ages 40 and 44, and then again in the 50s and 60s. Ulcerative colitis is a chronic disease which tends to get worse over time. The cause of ulcerative colitis is unknown. There may be a genetic underlying abnormality as 8%-14% of cases occur in a person who has an affected family member. Having a first-degree relative with ulcerative colitis increases your risk of developing UC by a factor of four. The prevalence of ulcerative colitis is highest in the Jewish population and black people. It is less common in those of Asian descent. The prevalence is the same in males and females.”
Ulcerative colitis: Diagnosis
A review in the journal of Gastroenterology Clinics of North America recommends an endoscopy as the best course to diagnose ulcerative colitis, although laboratory and radiographic findings may also help.
Dr Perry tells us that bloody stool is always a reason to visit the doctor. “If you’re experiencing frequent periods of diarrhea and tummy pain, or notice blood in the stools then it’s best to book an appointment as soon as possible with your GP,” he says. “They will normally suggest some blood tests and take a stool sample to determine the problem and help to reach a diagnosis.”
Dr Lee tells us some of the other tests that may also be necessary:
- A plain abdominal X-ray or abdominal CT scan to get a detailed picture of your colon and rectum.
- A sigmoidoscopy: this is a telescope passed up inside the back passage to directly visualize the bowel wall and enable biopsies (small pieces of tissue) to be taken.
- A colonoscopy: again, this is a test in which a thin tube containing a camera is passed right around the colon. A bowel prep is needed to empty the bowel in advanced, and the process is conducted under light sedation.
Ulcerative colitis: Treatment
A review in the Nutrients journal found that diet can be an effective tool in the management of ulcerative colitis, although more research into the area is needed. A 2016 study in the European Journal of Gastroenterology and Hepatology tested colitis patients during a disease flare-up over 4-6 weeks, and 69% of patients claimed they found dietary advice moderately or significantly helpful in the management of their symptoms.
Dr Perry explains that depending on the type of ulcerative colitis you have, you may be offered different treatments. “Depending on the severity, most GP’s will recommend medicine such as Aminosalicylates, corticosteroids or immunosuppressants,” he says. “For others, such is the severity that they may have to be admitted to hospital for treatment where possible colon surgery can be discussed. It’s advised regardless to follow a healthy eating diet, and most sufferers find that high fiber foods can cause flare-ups and make the condition worse.

“Nuts and seeds, spicy foods, alcohol, caffeine, dairy and certain vegetables have also been seen to be more problematic. However, it’s not advised to cut out all of these food groups. Try to keep a food diary and see when flare-ups are happening, and cut these foods out in the short term to see if it makes a difference.”
A review in the journal of Current Clinical Pharmacology found that prebiotics and probiotics may be effective in the induction and maintenance of remission in those with ulcerative colitis, although more structured clinical studies need to be undertaken to confirm this.
Dietary changes might be needed for those suffering with ulcerative colitis in order to manage their symptoms. Dr Lee says these may include:
- Eating 4-6 small meals a day.
- Keeping yourself properly hydrated. You can tell if you are well hydrated if your urine is pale yellow to clear. You can drink water or anything that helps improve your fluid balance such as soup, or fruit juice.
- Sipping slowly and often, using a straw if needed. Don’t gulp as this tends to result in swallowed air.
- Planning your meals and sticking to foods you like to eat.
- Cooking simply: steam, boil or poach, rather than going for fried or roasted food.
- Keeping a food diary so you can see what you were eating if symptoms are good, or bad, and make sensible alterations.
She also explained that an elimination diet may be necessary if your symptoms continue: “You may be advised to go on an elimination diet if you have a flare-up. This is only done with medical supervision,” she says. “The aim is to identify any trigger foods which could exacerbate your symptoms. Trigger foods might include high-fiber foods, foods containing lactose, certain types of sugars such as sorbitol or mannitol, sugary foods such as cakes and pastries, high-fat foods, alcohol and spicy foods.”
This article is for informational purposes only and is not meant to offer medical advice.
Additional resources
- To learn how you can participate in clinical trials for ulcerative colitis, go to http://www.nih.gov/health/clinicaltrials.
- Read more about ulcerative colitis at diagnosis and treatment at the American Family Physician.
- The National Health Service in the United Kingdom has some helpful descriptions of treatments for ulcerative colitis.

Lou Mudge is a health writer based in Bath, United Kingdom for Future PLC. She holds an undergraduate degree in creative writing from Bath Spa University, and her work has appeared in Live Science, Tom's Guide, Fit & Well, Coach, T3, and Tech Radar, among others. She regularly writes about health and fitness-related topics such as air quality, gut health, diet and nutrition and the impacts these things have on our lives.
She has worked for the University of Bath on a chemistry research project and produced a short book in collaboration with the department of education at Bath Spa University.
 Live Science Plus
Live Science Plus