Veins and arteries: Facts about our blood vessels
The expanse of veins, arteries and capillaries underneath the skin keep our cells energized and healthy.
Veins, arteries and other blood vessels are essential to our body's survival. To deliver blood around the body, a sophisticated circuit of blood vessels provides oxygen, removes waste, and maintains pressure so that the vascular network can operate ceaselessly.
Every cell in the human body requires oxygen to produce energy, but most of our cells cannot access it directly. A single–celled life form interacts directly with its environment, exchanging nutrients and waste products as required, according to the journal Environmental Microbiology Reports. But our ancestors gave up that lifestyle hundreds of millions of years ago when they evolved to become multicellular.
As this multicellular life grew more sophisticated, our ancestors' cells became specialised and compartmentalized, according to NASA.
Many millions of years later, their descendants migrated from the ocean to the land. Instead of external cells exchanging nutrients with their environment, our ancestor's cells were encased inside a protective barrier of skin, enabling them to retain their water and maintain consistent internal temperatures. This meant that precious few cells interacted with the environment, and therefore precious few cells could access much–needed oxygen and sugars for energy.
Fortunately, our species, just like our land–treading ancestors, possesses an interwoven network of tissues and organs dedicated to ensuring our cells acquire the nutrients that they need, according to the book "Regulation of Tissue Oxygenation" (Biota Publishing, 2011). We call this network the circulatory system.
The vascular network
The circulatory system is comprised of a pump — the heart — and a connected network of blood vessels that carry blood to and from internal tissues. If blood and its component parts are the delivery service, busily dispensing oxygen and collecting waste, then blood vessels are the highways and smaller roads on which they travel.
Together with the heart, which provides the pressure that propels blood around the circuit in the body, blood vessels are essential for maintaining the health and functionality of our cells.
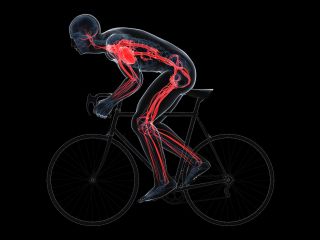
Our circulatory system is also highly adaptable, according to the journal Comprehensive Physiology. When we're at rest and require less energy, the heart rate slows. However when we move about and exercise the heart rate rises. To feel the beating heart in action for yourself, you can place a finger on the left side of your wrist, or next to the left side of your windpipe.
When doing this, you feel your pulse through the radial and carotid arteries.
As well as the heart, blood vessels themselves react to environmental changes. When it is cold for example the blood vessels constrict, helping to reduce heat loss.
The reverse is also true, as blood vessels expand when it is hot to help our bodies shed excess heat. Therefore, as well as supplying the body with nutrients, our vascular network helps regulate our internal environment, helping to both fuel and protect our cells.
The circulatory system
Types of blood vessels
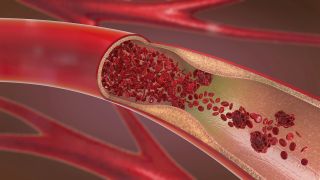
For blood to efficiently migrate throughout and around the body it must maintain optimal levels of pressure. Oxygenated blood from the left side of the heart is pumped outward at high pressure, therefore arteries must be able to withstand and maintain this force.
They withstand pressure by possessing a thick, muscular wall consisting of an outer, middle, and inner layer; and they maintain pressure by possessing a narrow lumen (the space that the blood travels through), according to the journal Hypertension.
Elastic arteries, which are found near the heart muscle, possess more elastic tissue in their middle layer. This helps convert the incremental pulses of pressure resulting from heart beats into a more constant pressure. Capillaries are also highly pressurised, but on a much smaller scale.
Their lumens are very narrow and their cells walls only one–cell thick. Veins, in contrast, also possess three layers in their walls, but these are much thinner while their lumens are much wider, yielding lower pressures.
Common diseases
In the U.K., diseases affecting blood vessels are amongst the biggest killers each year, according to the British Heart Foundation. The cells of our body are so dependent on the oxygen and nutrients supplied by blood that a blockage or a rupture in the vascular network can quickly cause catastrophic damage.
While some diseases are genetic, many common diseases are caused at least in part by lifestyle choices such as a poor diet, which results in the bloodstream carrying more harmful compounds than it ideally should. With an increasingly high–fat and sedentary lifestyle these diseases are growing ever more frequent. Fortunately, however, lifestyle changes and medical innovations are helping to save lives.
The heart requires a supply of blood to fuel itself. However, rather than gaining nutrients and oxygen from oxygenated blood, pumped in and out of its internal chambers, the heart muscle relies on coronary arteries wrapped around its exterior for its blood supply.
Over time, components transported by the blood such as cholesterol can stick to the walls of coronary arteries, initiating blockages that can partially or completely block the blood supply to parts of the heart.
This process is known as atherosclerosis and can result in angina, which is chest pain caused by insufficient blood supply to the heart. If coronary arteries are fully blocked, however, cell death of part of the heart can occur and cause a heart attack. Coronary artery disease can be treated using bypass graft surgery, where arteries are rerouted to supply the regions of the heart cut–off by coronary artery blockages.

Atherosclerosis describes the accumulation of plaque on arterial walls. These may originate at various places throughout the body but can become dislodged and carried elsewhere in the bloodstream. Eventually they can become stuck and cause a blood clot, blocking the artery and preventing blood flow to tissues and organs.
If this blood clot occurs in the arteries that feed the brain it can cause an ischaemic stroke, according to the American Stroke Association. After being deprived of oxygen brain cells very swiftly begin to die, causing numerous symptoms relating to the areas controlled by the affected region of the brain.
If one side of the brain is damaged, the opposite side of the body shows symptoms, which can include drooping of one side of the face, numbness in the corresponding arm, and slurred speech. Ischaemic strokes, if treated quickly, can be combated with medications that dissolve the blood clot, helping to restore blood supply to the brain.
A narrowing or hardening of artery walls can prove fatal when affecting organs such as the heart or brain, according to the Cleveland Clinic, but obstructed arteries feeding the peripheral organs can go unnoticed until the disease is at an advanced stage.
Depleted blood flow to the legs can cause symptoms such as cramping, an absence of hair, and gangrene that occurs following cell death. Individuals living with diabetes are at particular risk of developing peripheral arterial disease due to the abundance of glucose in blood plasma, which interferes with other components in the blood leading to plaque formation. However, a healthy lifestyle involving regular exercise, not smoking, and a low–fat, high–fiber diet can help prevent arterial disease for most adults.
Blood clots can result from plaques formed over long periods of time, but they can also appear rapidly in veins where blood flow is slow and laboured, which is most common in veins deep in leg muscle.
During these cases, such as when a person's legs remain unmoved for long periods on a flight, an excess of natural clotting factors in the bloodstream can overstimulate the production of a blood clot. In healthy blood, clots form to prevent bleeding, but during deep vein thrombosis the formed clot can grow to a substantial size large enough to obstruct blood flow.
This can cause pain, swelling, and a change in the color of the leg. However, according to the Mayo Clinic, the clot can cause yet more damage if it travels further through the vascular network into the vessels supplying the lungs, resulting in a pulmonary embolism which can prove fatal.
Additional resources
For more illustrations, of the upper and lower body circulatory system, you can visit the Cleveland Clinic website. To learn more about the difference between arteries and veins, watch this informative video from the Khan Academy.
Bibliography
- "Macroecology of unicellular organisms – patterns and processes". Environmental Microbiology Reports (2011).
- "How Did Multicellular Life Evolve?". Astrobiology at NASA (2017).
- "Regulation of Tissue Oxygenation" (Biota Publishing, 2011)
- "Cardiovascular Adaptations to Exercise Training". Comprehensive Physiology (2015).
- "Arterial Wall Hypertrophy and Stiffness in Essential Hypertensive Patients". Hypertension (1995).
- "Facts and figures". British Heart Foundation (2022).
- "Atherosclerosis and Stroke". American Stroke Association (2021).
- "Coronary Artery Disease". Cleveland Clinic (2021).
- "Pulmonary embolism". Mayo Clinic (2020).
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
James Horton holds a PhD in evolutionary biology from the University of Bath in the U.K. and has been writing about science since 2016. His work has been featured in The Conversation UK and BBC Future, and he’s been an interviewee on Spark podcast on Canadian Broadcasting Corporation. James currently works as a research scientist where he studies the causes of mutations and how these processes shape the evolution of bacterial genomes.

