Leading ingredient in over-the-counter decongestants doesn't work, FDA panel rules
The Food and Drug Administration reviewed data on phenylephrine, an ingredient in many popular decongestants, and deemed it ineffective when taken orally.
Get the world’s most fascinating discoveries delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?

Delivered Daily
Daily Newsletter
Sign up for the latest discoveries, groundbreaking research and fascinating breakthroughs that impact you and the wider world direct to your inbox.

Once a week
Life's Little Mysteries
Feed your curiosity with an exclusive mystery every week, solved with science and delivered direct to your inbox before it's seen anywhere else.

Once a week
How It Works
Sign up to our free science & technology newsletter for your weekly fix of fascinating articles, quick quizzes, amazing images, and more

Delivered daily
Space.com Newsletter
Breaking space news, the latest updates on rocket launches, skywatching events and more!

Once a month
Watch This Space
Sign up to our monthly entertainment newsletter to keep up with all our coverage of the latest sci-fi and space movies, tv shows, games and books.

Once a week
Night Sky This Week
Discover this week's must-see night sky events, moon phases, and stunning astrophotos. Sign up for our skywatching newsletter and explore the universe with us!
Join the club
Get full access to premium articles, exclusive features and a growing list of member rewards.
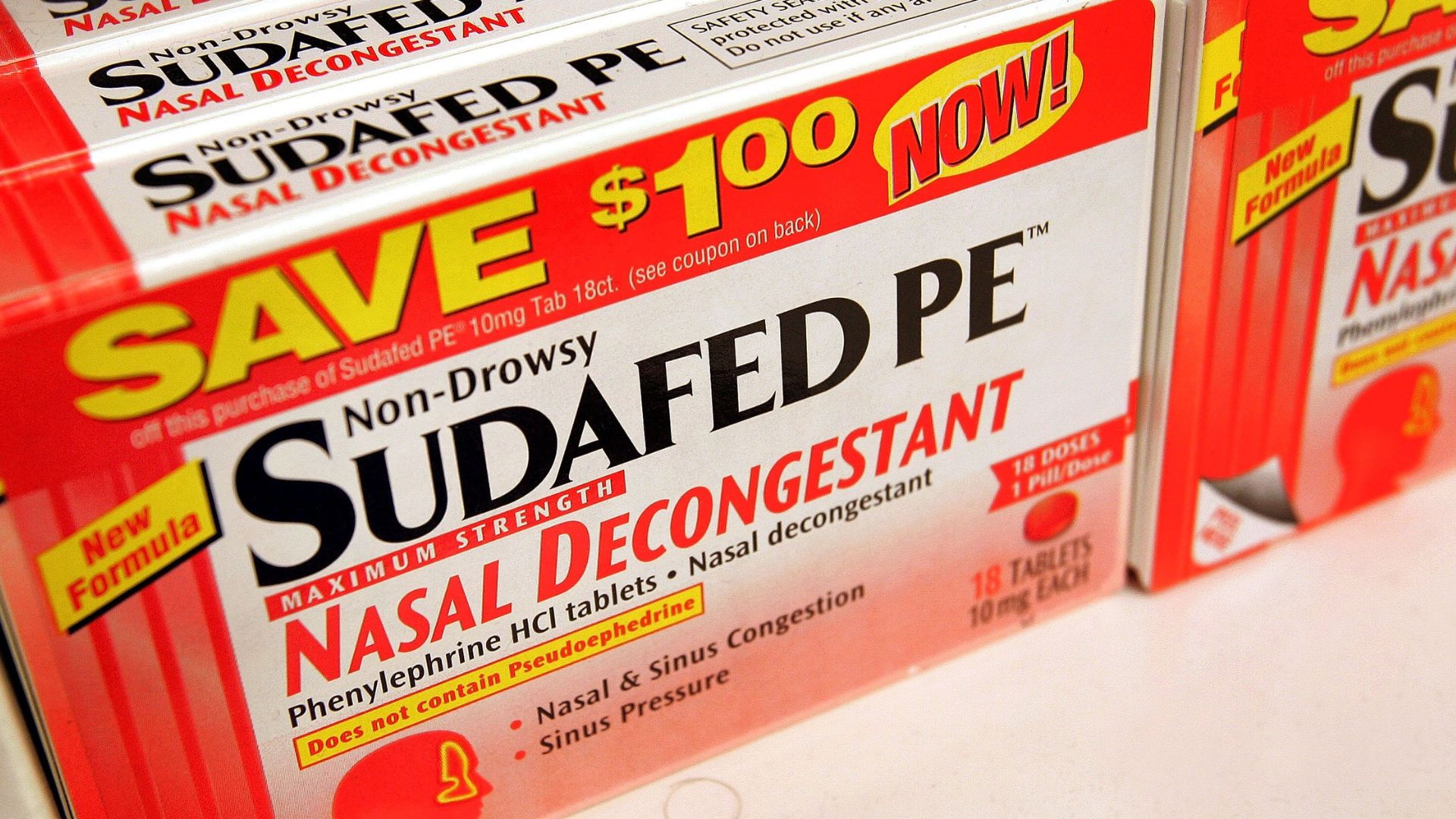
A key ingredient in popular decongestants such as Sudafed PE, Benadryl Allergy Plus Congestion and DayQuil Cold & Flu doesn't relieve nasal congestion when taken orally, a Food and Drug Administration (FDA) panel concluded in a meeting Tuesday (Sept. 12).
After reviewing years' worth of data, the FDA's Nonprescription Drug Advisory Committee (NDAC) found that the effectiveness of the decongestant ingredient, phenylephrine, can help relieve a stuffy nose when delivered straight into the nose — via a nasal spray, for example — but doesn't work when taken by mouth, the 16 panelists unanimously decided.
That's because, when taken orally, less than 1% of the drug actually ends up in the bloodstream and thus reaches the tissues of the nose that it's supposed to help, the committee reported in a memo from the meeting. (Phenylephrine is supposed to work by constricting blood vessels in the nose and sinuses.)
Related: What are amphetamines?
So, if they don't work, how did phenylephrine-based pills get approved in the first place?
"The bottom line is that none of the original studies stand up to modern standards of study design or conduct," Dr. Peter Starke, an FDA official who led the review, told The Associated Press. Past studies of the drug had inconsistent results and too-small sample sizes, and they relied on outdated statistical methods and technology that the regulators would no longer accept, Starke and his colleagues concluded.
Phenylephrine was first evaluated as an over-the-counter oral and intranasal decongestant back in 1976, according to the NDAC memo. But the ingredient gained popularity in 2005 as a substitute for pseudoephedrine, a different decongestant that had been moved behind the counter by a law intended to rein in the sale of drugs that can be used to make meth.
Get the world’s most fascinating discoveries delivered straight to your inbox.
Because of this, phenylephrine soon became commonplace in over-the-counter decongestants, and now, it's the most popular decongestant in the U.S., NBC reported. Despite its popularity, though, the ingredient's effectiveness has long been debated.
In 2007, after new formulations of popular decongestants started rolling out, University of Florida researchers petitioned the FDA to review the drug's effectiveness in adults. The researchers provided some evidence that the oral formulas were ineffective, but the FDA advisers responded by saying they still needed more data. Since 2007, three large clinical trials of oral phenylephrine have been conducted.
"These three trials represent by far the largest and most carefully constructed trials that have ever been performed to evaluate the decongestant effect of oral PE [phenylephrine]," the NDAC memo states. The trials showed that the drug had no more effect than a placebo, and additional data from the FDA's clinical pharmacology lab showed very little of it enters the bloodstream.
"We believe that these new clinical pharmacology and clinical data are consistent, substantial, and believable, and they confirm that orally administered PE is not effective at any dose that can be developed and still provide a reasonable margin of safety," the NDAC stated.
With the NDAC's evaluation done, the FDA must now decide whether to revoke phenylephrine's designation as "generally recognized as safe and effective." If it loses that designation, over-the-counter products containing the drug would likely need to be removed from shelves and reformulated by suppliers, according to NBC.
Editor's note: This story was updated on Sept. 13 to correct an error that stated Allegra-D contains phenylephrine; it contains pseudoephedrine. The article was first published on Sept. 12.

Nicoletta Lanese is the health channel editor at Live Science and was previously a news editor and staff writer at the site. She holds a graduate certificate in science communication from UC Santa Cruz and degrees in neuroscience and dance from the University of Florida. Her work has appeared in The Scientist, Science News, the Mercury News, Mongabay and Stanford Medicine Magazine, among other outlets. Based in NYC, she also remains heavily involved in dance and performs in local choreographers' work.
 Live Science Plus
Live Science Plus










