Study: Stem Cells Reverse Paralysis in Rats
Transplanted adult stem cells have been found to reverse paralysis associated with spinal cord injuries in lab rats, a new study finds.
The study, headed up by Miodrag Stojkovic, deputy director and head of the Cellular Reprogramming Laboratory at Centro de Investigacion Principe Felipe in Spain, involved transplanting so-called progenitor stem cells from the lining of rats' spinal cords into rodents with serious spinal cord injuries.
The rats recovered significant motor activity one week after injury, Stojkovic and his co-authors wrote in the Jan. 27 early online edition of the journal Stem Cells.
Spinal cord injury, for which no therapy currently exists to undo the damage, is a major cause of paralysis. Up to 400,000 people in the United States are estimated to live with these injuries, according to the Christopher and Dana Reeve Foundation. Most spinal cord injuries are caused by vehicle crashes and falls, and most of those injured are males.
The researchers say the new rat results "open a new window on spinal cord regenerative strategies."
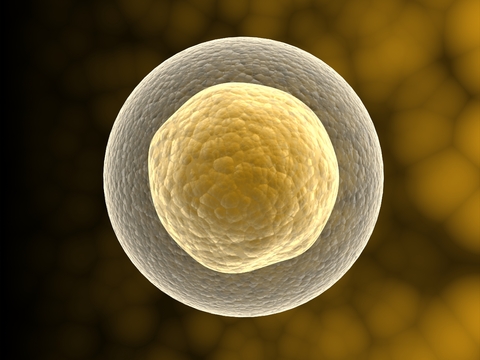
The rat study involved adult stem cells, which are found in adult tissues. It is the other type of stem cells, embryonic stem cells, that some activists find objectionable, partly because these cells are derived from embryos though a process that currently destroys them.
Last week, there was big news related to embryonic stem cells. The Food and Drug Administration approved the first study to inject human-derived embryonic stem cells into individuals with acute spinal cord injuries.
Get the world’s most fascinating discoveries delivered straight to your inbox.
The Bush Administration had placed restrictions on federal funding for new lines of embryonic stem cells for research, but the cells to be used in the study are old ones that would still have been eligible for funding in the Bush era. It is expected that President Obama will lift the restrictions.
Cells proliferated
The newly transplanted progenitor cells, which had been taken from the injured rats after spinal cord injury, were found to proliferate and were recruited by the specific injured area, Stojkovic said. The transplanted cells regenerated 10 times faster while in the transplant subject than similar cells derived from healthy control animals.
The trauma associated with spinal cord injury destroys numerous cell types, including the neurons that carry messages between the brain and the rest of the body. In many spinal injuries, the cord is not actually severed, and at least some of the signal-carrying nerve cells remain intact. However, the surviving nerve cells may no longer carry messages because oligodendrocytes, which comprise the insulating sheath of the spinal cord, are lost.
The regenerative mechanism discovered was activated when a lesion formed in the injured area. After a lesion formed in the transplant subject, the stem cells were found to have a more effective ability to differentiate into oligodendrocytes and other cell types needed to restore neuronal function.
"This answers one question: is the adult organism capable of regenerating neurological dysfunction following injury? Our present experimental data strongly support that this is the case: the spinal cord contains functional regenerative machinery," Stojkovic told LiveScience.
Previous attempts to transplant stem cells to reverse paralysis were based on spinal cord-derived stem cells from either fetal or healthy adult donors. These efforts reported only modest or no significant functional improvement soon after transplantation, Stojkovic said.
Human potential
The presence of these stem cells in the adult human spinal cords suggests that stem cell-associated mechanisms might be exploited to repair human spinal cord injuries.
Given the serious social and health problems presented by diseases and accidents that destroy neuronal function, there is an ever-increasing interest in determining whether adult stem cells might be utilized as a basis of regenerative therapies.
"The human body contains the tools to repair damaged spinal cords. Our work clearly demonstrates that we need both adult and embryonic stem cells to understand our body and apply this knowledge in regenerative medicine," Stojkovic said.
The research was funded by the Spanish Program of Regenerative Medicine, Conselleria de Sanidad de la Generalidad Valenciana-Instituto de Salud Carlos III, Fondo de Investigaciones Sanitarias-Instituto de Salud Carlos III and the Ministerio de Educacion, Ciencia y Tecnologia.
- Stem Cells Could Replace Plastic Surgery
- Video – Seeing Machine Helps Restore Eyesight
- 5 Things You Should Know About Stem Cells