Viruses Could Target Hard-to-Kill Cancer Cells
For the first time, researchers have shown viruses can be delivered through a person's bloodstream to infect cancer cells without infecting other tissues, according to a new study.
Once inside a tumor cell, the genetically engineered virus can replicate and spread to other cancer cells while it leaves normal cells alone. In the study, patients experienced few side effects.
The results mean that "we have new approach to cancer treatment that would be much more selective" than current treatments, said study researcher John Bell, a senior scientist at Ottawa Hospital Research Institute in Canada. Such a treatment could be particularly helpful for treating metastatic cancers, which are cancers that have spread throughout the body.
The study was small, including just 23 patients, and as an early-stage clinical trial, it set a goal of testing the safety of the treatment rather than seeing whether the viruses could kill cancer cells or help patients live longer.
The researchers plan to conduct a larger study to test whether their therapy is more effective than current cancer treatments. "We will need to do more trials to know if this virus can truly make a difference for patients," Bell said.
The study will be published tomorrow (Sept. 1) in the journal Nature.
Targeting cancer
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
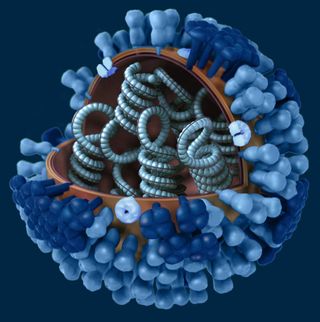
Cancer cells have defects that make them more susceptible than other cells to viral infections, Bell said. The researchers used a weakened strain of the vaccinia virus, the virus used in the smallpox vaccine.
Once inside a tumor cell, the virus, called JX-594, takes over the cell's machinery to replicate itself. The virus essentially becomes a parasite within the tumor cell and kills it, Bell said.
Other research groups are working on using other types of viruses to treat cancer, but none so far has been able to administer the virus into a patient's bloodstream and show, through an analysis of tissues from the patient, that the virus infected tumor cells and not other cells, the researchers said.
In the new study, patients received various doses of the viral therapy. The patients' cancers had been unresponsive to previous other treatments, and had become metastatic.
After eight to 10 days, the researchers biopsied the patients' tumors and surrounding tissues. The virus was engineered to carry a foreign gene so that the researchers could detect it.
Tissues from seven of the eight patients who received the highest doses showed that the virus was replicating in their tumors and not in normal tissues, the researchers said. Furthermore, six of these patients showed shrinkage or stabilization of their tumors, the researchers said. Those who received lower doses were less likely to experience tumor shrinkage or stabilization.
The most common side effect was mild to moderate flu-like symptoms that lasted less than one day, the researchers said.
Next steps
Dr. Miguel A. Villalona, director of the division of medical oncology at Ohio State University Medical Center, called the study a step forward in viral cancer therapy research.
"What this is showing is that, theoretically, they reliably can deliver genes into the tumor by using this virus," said Villalona, who was not involved in the study.
Villalona likened the therapy to sending astronauts to a space station. "What they are showing is that this may be a good shuttle," he said, but it is not yet known whether the shuttle can carry "astronauts." The next step would be to see if this virus can carry specific genes intended to kill the cancer, Villalona said.
The study was funded by Jennerex Inc., the company that makes JX-594, and was co-founded by Bell.
Pass it on: Viruses can specifically target tumor cells when delivered through the bloodstream.
This story was provided by MyHealthNewsDaily, a sister site to LiveScience. Follow MyHealthNewsDaily staff writer Rachael Rettner on Twitter @RachaelRettner. Like us on Facebook.

Rachael is a Live Science contributor, and was a former channel editor and senior writer for Live Science between 2010 and 2022. She has a master's degree in journalism from New York University's Science, Health and Environmental Reporting Program. She also holds a B.S. in molecular biology and an M.S. in biology from the University of California, San Diego. Her work has appeared in Scienceline, The Washington Post and Scientific American.
Most Popular

